Permission to speak
Determining strategies towards the development of
gay, lesbian, bisexual, transgender and intersex friendly
aged care services in Victoria.
Written by Dr Catherine Barrett, Dr Jo Harrison and Jane Kent
A Project of Matrix Guild Victoria Inc
in conjunction with
Vintage Men Inc
April 2009
Funded by the Reichstein Foundation
Enquiries and further information
• Jane Kent, Program Co-ordinator, Community Development Worker, Matrix Guild
Victoria Inc, inquiries@matrixguildvic.org.au/PO Box 99, Fairfield Victoria 3078
(www.matrixguildvic.org.au).
• Paul Bussey, President, Vintage Men Inc., vintagemen@yahoo.com.au/PO Box 6769,
600 St Kilda Road Central Victoria 8008 (www.geocities.com/vintagemen).
• Dr Jo Harrison, Jo.Harrison@unisa.edu.au.
• Catherine Barrett, Project Researcher: c.barrett@latrobe.edu.au.
For further copies of this or the
My People
report, go to (www.matrixguildvic.org.au) or
(www.geocities.com/vintagemen).
© Copyright Matrix Guild Victoria Inc. Published by Matrix Guild Victoria Inc
ISBN 978-0-646-51296-9
Permission to speak
3
_____________________________________________________________________
Acknowledgements
Matrix Guild Victoria Inc. and Vintage Men Inc. would like to thank the following
individuals, groups and organisations for their contributions to this program:
• The Reichstein Foundation for funding the projects
• The participants who generously shared their stories
• The Program Coordinator. Jane Kent
• The Program Researcher.
Dr
Catherine Barrett
Matrix Guild Victoria Inc and Vintage Men Inc would specially like to thank Dr Jo Harrison
and Dr Ruth McNair for their input into this report and their assistance with the project.
The Steering Committee including:
• Jane Kent, The Program Coordinator, Community Development Worker, Matrix
Guild Victoria Inc.
• Paul Bussey, President, Vintage Men Inc.
• Dr Ruth McNair, General Practitioner, The Carlton Clinic and Senior Lecturer, The
Department of General Practice, The University of Melbourne, Member of the
Australian Lesbian Medical Association Committee and Member of the Ministerial
Advisory Committee on Gay
and Lesbian Health.
• Lola McHarg, Admissions Officer, The Brotherhood of St Laurence
• Barbary Clarke, Victorian Gay and Lesbian Rights Lobby
• Associate Professor Anne Mitchell, Director, Gay and Lesbian Health Victoria
• Lyn Morgain, CEO, The ALSO Foundation
• Zoe Dunbar: Office Manager and Volunteer Coordinator ,
The ALSO Foundation
• Heather Birch, Former Chair of ALSO Foundation’s Senior Project Advisory
Committee, former member of Community Development Committee
• Lesley Walsh, CEO, Women’s Health East
• Sam Seamer, Former representative Women’s Health Information in the South East
• Joy Free, Researcher, Women’s Health West
• Dr. Rosie Crone, Consultant Geriatrician and representative of the Australian
Lesbian Medical Association
• Dr. Jo Harrison, School of Health Sciences, The University of South Australia
• Dr Catherine Barrett, Project Researcher and Community Liaison Officer, The
Australian Research Centre in Sex, Health and Society.
And others who gave their support. including:
The Victorian AIDS Council, The Australian Lesbian and Gay Archives, Lizzi Craig, The
Victorian Equal Opportunity & Human Rights Commission, The Gay and Lesbian Liaison
Unit and Elder Abuse Prevention Unit with the Victoria Police, The Australian Research
Centre in Sex, Health and Society, Julie Peters, JOY FM, Philomena Horsley, Caitlin Street.
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
4
_____________________________________________________________________
TABLE OF CONTENTS
ACKNOWLEDGEMENTS ................................................................................................................... 3
GLOSSARY OF TERMS ...................................................................................................................... 5
EXECUTIVE SUMMARY .................................................................................................................... 7
B
...................................................................................................................................... 7
ACKGROUND
S
O
:
T
GLBTI
............................................................................ 8
TAGE
NE
HE PERSPECTIVES OF
SENIORS
S
T
:
T
................................................ 10
TAGE
WO
HE PERSPECTIVES OF AGED CARE SERVICE PROVIDERS
C
...................................................................................................................................... 12
ONCLUSION
BACKGROUND ................................................................................................................................... 13
P
............................................................................................................................ 15
ROGRAM OUTLINE
THE PERSPECTIVES OF GLBTI SENIORS RECEIVING AGED CARE SERVICES ............. 19
T
GLBTI-
................ 23
HE COMPONENTS OF
FRIENDLY AGED CARE SERVICES IDENTIFIED IN STAGE ONE
STAGE TWO: THE PERSPECTIVES OF AGED CARE SERVICE PROVIDERS .................... 26
D
............................................................................................................................. 26
ATA COLLECTION
F
:
T
............................................................................ 29
INDINGS
HE CONTEXT OF AGED CARE SERVICES
T
......................................................................................................... 48
HE SIGNIFICANCE OF CONTEXT
STRATEGIES TO CREATE GLBTI-FRIENDLY AGED CARE SERVICES ............................. 49
1.
T
......................................................................................... 49
HE IMPORTANCE OF POWERFUL ALLIES
2.
T
.................................................................... 51
HE IMMEDIATE NEED FOR ADVOCACY AND SUPPORT
2.
T
............................................................... 52
HE NEED TO EDUCATE AGED CARE SERVICE PROVIDERS
4.
T
................................................................................................. 56
HE ROLE OF CHANGE CHAMPIONS
5.
T
.......................................................................... 58
HE OPPORTUNITY TO EDUCATE THE COMMUNITY
6.
T
GLBTI
.................................... 58
HE OPPORTUNITY TO EMPOWER
SENIORS AND THEIR ADVOCATES
7.
T
GLBTI-
.................................................................. 61
HE VALUE OF
SPECIFIC AGED CARE SERVICES
8.
T
.................................................................................................... 63
HE SIGNIFICANCE OF RESEARCH
9.
T
............................................................................................... 64
HE SIGNIFICANCE OF LEGISLATION
C
........................................................................ 65
ONCLUSIONS REGARDING STRATEGIES FOR CHANGE
CONCLUSION ..................................................................................................................................... 66
A
1:
C
GLBTI
.............................................................. 67
PPENDIX
ORE ISSUES IN RELATION TO
SENIORS
A
2:
M
........................................................................................... 68
PPENDIX
EDIA INTEREST REGISTER
A
3:
L
....................................................................................................... 69
PPENDIX
IST OF RESOURCES
DRAFT STRATEGIC OPTIONS TO ENCOURAGE THE DEVELOPMENT OF GLBTI-FRIENDLY
AGED CARE SERVICES IN VICTORIA ......................................................................................... 71
1.
E
...................................................................................................... 71
STABLISH A LOBBY GROUP
2.
D
............................................. 72
EVELOP PROCESSES FOR IMMEDIATE ADVOCACY AND SUPPORT
3.
E
............................................................................... 72
DUCATE AGED CARE SERVICE PROVIDERS
4.
S
.................................................................................................. 76
UPPORT CHANGE CHAMPIONS
5.
E
....................................................................................................... 76
DUCATE THE COMMUNITY
6.
E
GLBTI
................................................................. 76
MPOWER
SENIORS AND THEIR ADVOCATES
7.
S
GLBTI-
.................................................... 77
UPPORT THE DEVELOPMENT OF
SPECIFIC SERVICES
8.
C
................................................................................................. 77
ONDUCT FURTHER RESEARCH
REFERENCES ..................................................................................................................................... 78
TABLES AND FIGURES
T
2:
P
1
..................................................................................................... 20
ABLE
RÉCIS FROM CASE STUDY
T
3:
P
2
..................................................................................................... 21
ABLE
RÉCIS FROM CASE STUDY
T
4:
P
3
..................................................................................................... 22
ABLE
RÉCIS FROM CASE STUDY
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
5
_____________________________________________________________________
Glossary of terms
Aged care services:
Care provided for seniors including: (a) in their home such as
community nursing; domestic assistance; personal care; meals on wheels; home maintenance;
transport, and community-based respite care; (b) community services provided in community
centres; day-care centres; day hospitals; medical centres; (c) residential aged care services
such as nursing homes and hostels.
Bisexual
: A man or woman who is sexually and emotionally attracted to both men and
women.
Closet
: An historical term used to describe non-disclosure of sexual/gender identity.
Cross-dresser:
A person who dresses in clothes typical of the opposite sex.
Gay
: A man whose primary sexual attraction is towards other men.
Gender
: The socially defined roles assigned to males and females.
Gender identity:
a person’s own sense of identification as male or female.
GLBTI
: An acronym for gay, lesbian, bisexual, transgender and intersex.
Heterosexism
: Bias towards heterosexuals which ignores the presence and the needs of gay
men, lesbians and bisexuals.
Heterosexual
: A person whose primary sexual and emotional attraction is towards the
opposite sex.
Hostel
: residential aged care service for people with low level needs. Also referred to as ‘low
care’.
Homo/transphobia
: A dislike of people who are homosexual or transgender that may
manifest as discrimination or violence.
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
6
_____________________________________________________________________
Intersex
: A person born with sex chromosomes, external genitalia, or an internal
reproductive system that is not exclusively male or female.
Lesbian
: A woman whose primary sexual/emotional attraction is towards women.
Non-heterosexual:
A person who is gay, lesbian or bisexual (also know as queer).
Nursing home
: Residential aged care facility for people with high level of needs. Also
referred to as ‘high care’.
Out
: The disclosure of sexual/gender identity.
Residential aged care facility:
Nursing home and hostels which provide permanent
residential or respite care.
Senior
: A person 65 years or older.
Sexual identity:
A person’s identity, an established mental picture of self, can be a specific
and fixed sexual identity, although this can also be somewhat fluid. e.g., heterosexual,
homosexual, lesbian or bisexual.
Transgender:
refers to individuals who do not identify with the gender assigned to them at
birth. The terms male-to female and female-to-male transgender persons are used to refer to
individuals who are undergoing or have undergone a process of gender affirmation.
Transsexual:
A transgender person who is in the process of seeking, or has successfully
completed, sexual reassignment surgery.
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
7
_____________________________________________________________________
Executive summary
This is the report from Stage Two of a Matrix Guild Victoria and Vintage Men research
project.
The report from Stage One,
My People: A project exploring the experiences of Gay, Lesbian,
Transgender and Intersex seniors in aged-care services
is available online at
www.matrixguildvic.org.au
and
www.geocities.com/vintagemen
Background
Stage one of the project revealed that many gay, lesbian, bisexual, transgender and intersex
(GLBTI) seniors do not feel safe disclosing their sexual or gender identity in aged care
services. This is not surprising, given that many of these men and women grew up in an era
when disclosure could result in imprisonment, enforced medical ‘cures’, loss of employment
and rejection by family and friends. However, the decision to hide one’s sexual/gender
identity in aged care services is also reinforced by recent anecdotal reports of discrimination
when disclosure occurs.
One of the consequences of closeting, or hiding one’s sexual/gender identity is that aged care
service providers are unaware of GLBTI clients and their particular needs. This invisibility,
and the lack of evidence regarding the experiences of GLBTI seniors, perpetuates the status
quo in which discrimination often goes unchallenged. Aged care service providers are also
often unaware of the importance of providing GLBTI-friendly services.
Aged care service providers may also be unaware of their legal r esponsibilities in relation to
GLBTI seniors. The Victorian Equal Opportunity & Human Rights Commission (2006)
identifies that the human rights of all Australians, including GLBTI seniors receiving aged
care services, are recognised. In particular, under the
Charter of Human Rights and
Responsibilities
(2006), public agencies are obliged to consider that people have the r ight to
enjoy their human rights without discrimination and the right to enjoy their identity and
culture. Additionally, the
Equal Opportunity Act
(1995) makes it
unlawful to discriminate
against someone on the basis of her or his sexuality or gender, including discrimination in the
provision of goods and services such as
aged care services. Furthermore, the
Statute Law
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
8
_____________________________________________________________________
Amendment (Relationships) Act
(2001) recognises that people in same-sex relationships have
the same rights as heterosexual couples to authorise medical treatment and access information
about their partner’s health and hospital visitation.
To assist aged care services to achieve the necessary reforms, Matrix Guild Victoria Inc., in
conjunction with Vintage Men Inc., developed a four-stage Program for aged care services in
Victoria. The overall aim of the Program is to reduce disparities for GLBTI seniors in aged
care. The first two stages of the Program, which conclude with the publication of this report,
explored the experiences of GLBTI seniors in aged care services and the perspectives of aged
care service providers in order to provide a catalyst for change. The additional Program
stages aim to support the development of GBLTI friendly services.
Stage One: The perspectives of GLBTI seniors
Stage one of the Program, conducted in 2007, included two phases to explore the experiences
of GLBTI seniors in aged care services. The
first phase
involved in-depth interviews which
explored the experiences of GLBTI seniors receiving aged care services. The
second phase
involved extending interviews to inform the construction of case study narratives.
Participants were invited to describe: their perceptions and/or experiences of being GLBTI in
the early twentieth century; their needs as a GLBTI senior; their experiences disclosing
sexual/gender identity; any positive or discriminatory experiences of aged care services; the
impacts of aged care services on their lives; and any changes required to enable seniors to
feel safe disclosing their sexual/gender identity. Interviews were audio-recorded and
participants verified interview notes before a thematic analysis was conducted.
Interviews were conducted with 25 participants. The stage one study clarified that some
GLBTI seniors are exposed to discrimination in aged care services. The study also identified
strategies to address this issue. Firstly, participants expressed their support for GLBTI-
specific aged care services. Secondly, the need for staff education related to the needs of
GLBTI seniors was also identified.
The need for the education of aged care service providers was explicitly described by some
participants. That such education is imperative was also implied in the issues presented. Most
participants referred explicitly to the importance of ‘My people’. This referred to family,
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
9
_____________________________________________________________________
friends and aged care service providers with whom they could be themselves. Analysis of the
conversations around ‘My people’ highlighted five key characteristics that can be applied to
aged care service providers for the development of GLBTI-friendly aged care services. These
characteristics were understanding, empathy, trust, advocacy and leadership. The underlying
theme of understanding was pivotal to staff education around eight core issues identified as
follows.
Core issues for GLBTI seniors
1. The impact of historical experiences of discrimination:
The current generation of
GLBTI seniors was coming of age at a time when their sexual/gender identity could result
in enforced medical ‘cures’, imprisonment or loss of family, employment and friends.
Consequently, they have special needs which need to be understood by aged care service
providers.
2. Invisibility as an impact of current discrimination:
Some GLBTI seniors closet their
sexual/gender identity in aged care services and there are reasons behind this occurrence.
3. The impact of identity concealment:
GLBTI seniors who feel unable to disclose their
sexual/gender identity may: feel unable to be themselves and therefore feel devalued or
depressed; experience stress and pressure from maintaining a façade of heterosexuality;
have unmet care needs; and have limited opportunities for sexual expression.
4. The impact of inadvertent visibility:
Some GLBTI seniors are exposed to
discrimination from staff, co-clients and visitors because they are unable to hide their
sexual/gender identity.
5. The impact of dementia:
Some GLBTI seniors have dementia and need staff to
understand that the grief and loss involved in having a same-sex partner with dementia is
no less than that experienced by a heterosexual couple
6. Enabling sexual and cultural expression:
Sexual and cultural expression is important
for the mental health of GLBTI seniors in many respects.
7. Inadequate standards of care: Inadequate standards of care:
Some aged care services
discriminate against GLBTI seniors by failing to create GLBTI-friendly services.
8. Achieving a safe environment:
A positive response to the disclosure of sexual/gender
identity can result in GLBTI seniors feeling understood, valued and safe.
These themes were presented to aged care service providers in stage two to determine their
perspective and develop strategies to create GLBTI-friendly aged care services.
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
10
_____________________________________________________________________
Stage Two: The perspectives of aged care service providers
Stage two of the Program, conducted in 2008, included two phases to determine the
experiences of aged care service providers and strategies to create GLBTI- friendly aged care
services. The
first phase
involved conducting three focus groups with aged care service
providers. The
second phase
involved 16 interviews with aged care service providers who
were unable to attend focus groups. Participants were presented with the findings from the
My People
report. They were then invited to describe their experiences in caring for GLBTI
seniors and determine strategies to create GBLTI-friendly aged care services. Two focus
groups were audio-recorded and all participants verified interview notes before a thematic
analysis was conducted.
The focus groups were attended by a twenty aged care service providers. Focus group one
included a care co- ordinator, a diversional therapist, a physiotherapy assistant, division two
nurses (2) and personal care attendants (3). Focus group two involved the director of nursing
and chief executive officer of a private nursing home and the director of nursing for a private
hostel. The third focus gr oup involved representatives from nine community support agencies
and advocacy groups which provided seniors’ services. Phone interview participants included
a chief executive officer, director of nursing, geriatrician, academic, educator, division two
nurse, personal care attendant, division one nurses ( 2) and service managers/coordinators (7).
Participants worked predominately in the government section (12) in Melbourne (12) and
provided services in residential aged care (3), home and community care (8), aged care
assessment service (1) and GLBTI support and advocacy (4).
Seven themes relating to the aged care context emerged following data analysis.
The context of aged care services
1. Ageism, homo/transphobia and the community:
The homo/transphobic and ageist
views of aged care service providers were considered to reflect the views of the
community. However the dependency of GLBTI seniors on aged care services meant
that these views were more damaging when held by service providers.
Homo/transphobia in rural communities, family members and heterosexual seniors in
shared services were also reported to create obstacles for GLBTI seniors.
2. The question of
sexuality in aged care:
Aged care service providers considered that
their industry was prudish and conservative. Sexuality was understood to be about sex
and seniors were not expected to be sexual or sexually diverse. Sexual expression was
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
11
_____________________________________________________________________
regarded as problematic and management strategies aimed at eradicating sexual
expression included libido suppressants. A recurrent theme was the lack of permission
to speak about sexuality. This was reflected in the reported consequent need for change
to create GLBTI-friendly aged care services.
3. The unknown needs of GLBTI seniors:
Many aged care service providers did not
understand the needs of GLBTI seniors. There was a common perception that being
GLBTI was about ‘who you had sex with’ and seniors were not expected to have sex.
Consequently, seniors that were GLBTI were not considered to have special care needs.
However, there was a genuine interest in stories about and from GLBTI seniors and in
learning about their care needs.
4. The challenge of shared services:
Aged care service providers were aware of the
challenges for GLBTI seniors in shared services. However, the uncertainty around the
needs of GLBTI seniors created uncertainty for some aged care service providers
around how they could be supported in shared services. The balance of client rights and
responsibilities appeared to be clouded by the levels of comfort some staff had with
GLBTI seniors.
5. The value of change champions:
GLBTI service providers shared stories of
championing change by role modeling or advocating for particular clients. Having a
GLBTI member of staff appeared to be correlated with aged care service provider
comfort for GLBTI seniors. Some teams and organisations had significant numbers of
GLBTI staff and wer e renowned for providing leadership in the GLBTI community and
excellence in the care of GLBTI seniors. Several heart warming stories were told of
aged care service providers that had never met a GLBTI person but championed change
from a compassionate perspective. Others suggested reliance on organisational systems
rather than individual champions to ensure GLBTI seniors who disclosed their
sexual/gender identity were supported if a champion left the service.
6. Gay men and the fear of HIV/AIDS:
Aged care service providers reported a general
fear in the industry about gay men and the contagion of HIV/AIDS. These fears could
result in staff withdrawing physical contact from a gay senior. They could also result in
gay and/or HIV positive seniors choosing death rather than entering residential aged
care.
7. Fear of the unknown - transgender seniors:
Fear was also apparent in the
conversations around transgender seniors. These seniors appeared likely to receive a
negative response including in some rural areas where staff had never met a transgender
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
12
_____________________________________________________________________
person. Stories were shared of transgender seniors encountering discrimination from co-
clients in shared services and of cross dressers being prohibited from cross dressing.
Concerns were also expressed about the readiness of aged care service providers to
support transsexuals to maintain their gender identity.
Conclusion
This report presents the experiences of aged care services providers regarding GLBTI-
friendly aged care services in Victoria. The complimentary perspectives of GLBTI people
themselves and these service providers offers a str ong foundation for the future development
of an action plan to create GLBTI-friendly aged care services. No previous studies in
Australia have sought feedback from service providers and recipients to develop an action
plan to create GLBTI-friendly aged care services. The program has generated interest in the
media, discussion in the community and debate amongst aged care service providers and the
GLBTI community. This level of attention has increased the visibility of GLBTI seniors and
raised concerns about their experiences in aged care services. This increased awareness will
serve as the bedrock for the future development of policies, programs and services on the
ground which will reduce discriminatory experiences and enhance cultural competence.
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
13
_____________________________________________________________________
Background
You cop it sweet and shut up.
My family and I don’t talk because I’m gay and they disapprove.
Having ‘shock therapy’ was supposed to teach me how to be straight.
All it taught me to keep my mouth shut.
Some older women would be terrified of talking.
My brother said that I shouldn’t tell his children that I was having gender
reassignment surgery.
I couldn’t tell the staff that I’m gay.
People of his vintage didn’t really have the words to describe what was in them.
I keep my mouth shut. I have to be car eful what I say. I have no conver sation. I
can’t talk to the staff in here.
(Collage of quotes from conversations with GLBTI seniors).
We don’t even have language for it. We have to start the conversations.
There is a silence.
Some of the staff whisper and snigger.
They don’t talk about it. It’s not part of their lexicon.
We need to acknowledge our discomfort.
It requires constantly working with staff to say that it is OK to talk about it.
(Collage from conversations with aged care service providers).
In 2007 a pioneering study co-ordinated by Matrix Guild Victoria in
conjunction
with
Vintage Men ( Barrett, 2008) explored the experiences of gay, lesbian, bisexual and
transgender (GLBTI) seniors in aged care in Victoria. The study challenged decades of
silence around homo/transphobia in aged care services by presenting evidence that
discrimination occurred. The report, entitled
My People
, was r eported on and debated in the
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
14
_____________________________________________________________________
national and international media (see media interest register at Attachment 1) creating intense
interest in a group of people whose needs have been ignored for too long. The Australian
population is ageing and it is expected that by 2050 a quarter of the population will be aged
65 years and older (Australian Institute of Health and Welfare, 2002). While there are no
accurate figures on the percentage of seniors who are GLBTI
the proportion of the general
population that is not ‘exclusively heterosexual’ is thought to be between eight and eleven per
cent (Australian Medical Association, 2002) and increasing (Birch, 2004). The ageing of the
Australian population and the growing numbers of GLBTI people have contributed to the
growing interest in the experiences of GLBTI seniors.
The Australian Institute of Health and Welfare (2002b) has identified that, of Australia’s 2.4
million seniors (aged 65 and over), 42% need assistance to stay at home and around 5.2%
require permanent nursing- home or hostel care. The experiences of GBLTI seniors accessing
these and other aged care services are unique. For example, many were coming of age at a
time when homosexuality was illegal or considered to be a sickness from which they could be
cured. Consequently, many individuals ‘closet’ or hide their sexual identity to avoid
discrimination.
Recently, it has been recognised that as a result of their experiences of discrimination, GLBTI
seniors have special needs (Chamberlain and Robinson, 2002). However, given their history
of discrimination, many GLBTI seniors do not feel safe disclosing their sexual/gender
identity to aged care service providers and so their special needs are not always identified or
met.
Strategies for change involve promoting positive experiences of ageing and addressing
ageism and invisibility in the general community as well as the GLBTI community (Hughes
2007) and conceptualise sexuality as culture. In considering strategies to address issues in
Victoria, the challenge of aged care reforms has also been supported by Matrix Guild
Victoria Inc, a group founded to promote appropriate caring support for older lesbians,
combat ageism and advocate on behalf of older lesbians. Matrix Guild facilitates home-based
services for older lesbians, which involves organising the provision of services by
appropriately qualified lesbian
professionals for older lesbians who want to stay in their
home.
It has also conducted
two studies regarding the needs of older lesbians (Bryer, 2004)
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
15
_____________________________________________________________________
(Testro, 1997). Similarly, Vintage Men provides support to mature gay and bisexual men and
their friends, including pastoral care to those in residential aged care. The commitment of
Matrix Guild and Vintage Men to the needs of lesbian and gay seniors led to the development
of this Program.
Program outline
Matrix Guild was concerned about the anecdotal repor ts of discrimination affecting GLBTI
seniors in aged care services and thus identified the need to gather first-hand accounts of aged
care experiences which could serve as a catalyst for change. They worked in conjunction with
Vintage Men to develop a program that would promote the well-being of GLBTI seniors by
challenging their invisibility in aged care services.
The four stage program aims to support the well-being of GLBTI seniors in Victoria and
assist GLBTI seniors to feel safe disclosing their sexual/gender identity and ensure that their
needs are met. The four stages have been clearly identified, (see Figure 1). The first stage
gathered evidence of the experiences of GLBTI seniors in aged care services.
This report of the second stage seeks to determine strategies to enhance aged care services by
presenting the findings from stage one to aged care service providers and seeking feedback
on strategies for change. Stage three will involve lobbying state policy-makers, agencies,
private bodies, organisations and government departments with influence, such as the
Council on the Ageing, the Department of Health and Ageing and the Office of Senior
Victorians to support the required changes.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
16
_____________________________________________________________________
Figure 1. The Four Stage Project
P ro g ra m
A im s to r ed u ce d is p ar it ies
f or GLB TI s en io rs re ceiv ing
age d car e s e r vices
St age O ne
S ta ge Tw o
St age T hr e e
St ag e F ou r
A im : To exp lo r e t h e
A im : To de t er m ine
A im : To lo bb y t h e V ict o ri an
A im : To s up p or t ag ed car e
ex pe ri en ces o f GLB TI
s t r at egi es t o cre at e GLB TI-
Go ver n men t to s u pp o rt
s er vice s t o cre at e GLB TI-
s en io r s in age d car e
fr ie nd ly a ge d c ar e s e rv ices
cha ng e
fr ie nd ly a ge d- car e s er vice s
s e rv ices
P h as e On e
P ha s e T w o
P ha s e O n e
Ph a s e T wo
2 5 int e rvi ew s d es cr ib ing 19
To b e d et er m in ed
To be d et er m in ed
3 ca s e s t u die s wi th GLB TI
3 fo cu s gr ou p s wit h 20
P ho n e in t er vie ws w it h 16
ex pe ri en ces o f GLB TI
Sen io r s
a ge d ca r e s e rv ice pr o vid er s
a ge d ca re s e rvi ce p r ov ide r s
s en io rs
All stages of the Program are designed to create new understandings, generate responsive
action and to reinforce the importance of hearing the voices of GLBTI seniors. To achieve the
over-arching aim of reducing disparities for GLBTI seniors, this r eport shows how stage two
seeks to engage aged care stakeholders including service users, service providers,
organisational managers and policy makers. The engagement of service users provides
evidence which can increase the potential efficiency of change strategies, increase the interest
of service providers, create ownership of the issues identified (Barrett et al., 2005b) and assist
in questioning existing practices and beliefs (Bouras and Barrett, 2007). This engagement, in
conjunction with government consultation, can ensure support for sustainable change (Barrett
et al., 2005a). Given the importance of engaging stakeholders, the methods will be further
refined as the Program progresses to enable Program responsiveness to the stakeholder input.
The methods employed in stage two are described in the following section.
Credibility and trustworthiness
To maximise the value of the study’s findings, particular attention was paid to the
methodological approach employed in the research. The trustworthiness and authenticity of
the methods wer e considered to ensure that the study was credible, or did not contain
biased
distortion of data
(Patton, 2002). Authenticity is described as giving
direct expression to the
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
17
_____________________________________________________________________
‘genuine voice’, which ‘really belongs’ to those whose life-worlds are being described
(Winter, 2002). To promote genuine voices the participants in both stages were provided with
interview and focus group notes for verification. Increasing the trustworthiness of the study
by making the study practices visible (Sandelowski, 1993) was achieved by developing an
audit trail, or list of program records, providing a picture of what occurred (Kemmis and
McTaggart, 1982)
.
Ethical considerations
A study protocol highlighting the ethical considerations was developed for stage one and two
and reviewed by the Program Steering Committee. These documents complied with the
Australian Code for the Responsible Conduct of Research (National Health and Medical
Research Council, 2007). Ethical approval was also gained from the Victorian AIDS Council
Ethics Committee for stage one in relation to an interview with a client of their service. All
participants were provided with a plain-language statement describing the study and the
possible risks. These included the potential limits to confidentiality for focus group
participants. All participants signed a consent form before participating. Ethical
considerations included the need to protect confidentiality, and the possible vulnerability of
those
who were providing the critique of a service.
The following ethical considerations and strategies related to the focus groups. Participation
in the Project was voluntary and information sheets were provided to participants informing
them of possible risks from being in the stage two study. To ensure the ethical conduct of the
study a number of strategies were identified.
The first strategy related to the issue of confidentiality for focus group participants. In
particular, the confidentiality of comments made by focus group participants could not be
assured. All participants were informed that although comments made during the focus
groups should be kept confidential, it could be possible that participants repeat comments
outside of the group at some time in the future. Therefore, participants were encouraged to be
as honest and open as they could be, but to remain aware of limits in protecting
confidentiality.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
18
_____________________________________________________________________
To protect their identity, focus group participants were invited to introduce themselves to the
group using their first name or to use a pseudonym. Furthermore, to protect the identity of
their organisation participants were invited to describe the service they provided with out
naming the organisation or agency.
Most participants chose to de-identify their service and
themselves by using a pseudonym.
Also the recording of focus group interviews could contain information that may identify
participants. However, interviewees were told that this information would be checked to
ensure details such as participant names and organisation names were not included.
Participants were also invited to de-identify information before it was included in the project
report. It is also stated that it could be possible that in such group interaction participants may
feel peer pressure, embarrassment or discomfort with the views of others. They were told that
the facilitator would be mindful of this and would endeavour to create a discussion in which
diverse views were valued and expressed in a respectful manner.
The second strategy related to the potential for focus group participants to present a range of
views and experiences. It was stated that participants could be reluctant to express
homo/transphobic views given that the facilitator was employed by the Matrix Guild Victoria
Inc and that the Community Development Worker for the Matrix Guild would also be
present. However, it was stated and the facilitator would reiterate the importance of learning
from a range of views and experiences. The facilitator would also be aware that hearing such
a range of views may be challenging for participants, particularly if they are GLBTI
themselves.
Data analysis
This report presents the findings from stage two of the pr ogram. The focus of this stage was
the identification of issues that might inform strategies to create GLBTI-friendly aged care
services.
The principles which underpinned the process of collection and analysis of data throughout
both stages of the research are presented in the report from stage one
My People
. Matters of
methodological rigour are outlined, and commitment to credibility and trustworthiness as
aspects of the research approach is confirmed. The critical methodological approach, focused
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
19
_____________________________________________________________________
on the achievement of social justice, is outlined in reference to its application across the
qualitative research driven stages of the program. The process of collection and analysis of
data, including that the research took place within a context of commitment to ethical
practice, is elucidated.
As is outlined in the methods section of the stage one report, a process of thematic analysis
was applied to the data from interview and focus group transcripts, through a process of
identification of coding categories and codes so that specific themes could emerge. Findings
which were replicated or contrasted were identified (Yin, 2004) and presented to participants
for feedback.
The thematic analysis used the five stages of ‘framework’: familiarisation;
application of a framework; indexing; mapping; and interpretation (Ritchie and Spencer,
1994).
The perspectives of GLBTI seniors receiving aged care
services
To further explore the themes identified in stage one, précis from the case studies presented
in the stage one
My People
report are provided in the following tables. The first précis
presents the story of a gay man living with HIV/AIDS in a nursing home. The narrative is
presented by Tom and has been edited in collaboration with Lizzi, Tom’s Community
Support Officer from the Victorian AIDS Council. The second tells the story of Maureen who
cared for her partner Thelma at home with palliative care staff and home supports. The final
précis is told by Nancy, a transsexual woman in supported accommodation, and by Maggie
her carer.
The stories begin with a title selected by participants. The participants then speak for
themselves, with expletives and colloquialisms retained.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
20
_____________________________________________________________________
Table 1: Précis from case study 1
Why not take all of me?
My name is Tom and I have been in a nursing home since I had a stroke four years ago. I had the
stroke because I’ve got HIV. I’ve got two brothers and one sister, but we don’t talk because I’m
gay and I’ve got the HIV and they disapprove. I’ve got no-one in my life now that loves me.
Except the old girl, she loves me. When mum goes I’m done. Because I’m gay I’m a lonely man.
Oscar Wilde said: City life, millions of people living lonesome together.
When I came here I told the staff I was married and they started asking to see the pictures of my
wife. Of course I didn’t have any and because they knew I had HIV they worked out that I’m gay.
I can’t talk to the staff about being gay because I am worried my care will be worse. I’m not able
to live a gay man’s life here because there is no privacy, and there are rules and some people think
gay is disgusting. I keep my mouth shut. I have to be careful how I act and be careful what I say.
I’m only 64 but I am an old man. The HIV makes me feel old and this place makes me feel old.
I’ve got no-one to talk to here because the residents sleep all day and they have dementia. My
mind is still good, but I have no conversation. I talk to Lizzi; she’s my Community Support
Officer from the Victorian AIDS Council. I talk to her about how much I miss sex, touch and
intimacy but I can’t talk to the staff in here about that. When I realised there was nothing for me in
here; that I had to forget about a sexual relationship with a male, my libido was extinguished. For
a few years I rallied against this place, then I got depressed and I succumbed to it. I need to meet
interesting people to make me feel alive for a while. Then back to this deadness. What else is
there? I can’t talk to them. I am a reasonably intelligent man. It’s been depressing being in here so
I started antidepressants. They’re called happy pills. I had to go on them when I came in here, it’s
depressing.
I‘ve got extra services because of the HIV. People who know about HIV come here to help the
staff look after me. I have Lizzi who organises volunteers to take me out for a latte, a beer or a
drag show. They have helped with my HIV and they have changed the way staff treat me. See
they are used to gay men and I can be a gay man when I’m with them. They’ve educated staff
about how to care for me so I get better care. They check that I’m getting the right care. The staff
here know that there are people who are interested in what happens to me, that makes a difference.
The services that come in for my HIV have made some staff take interest in gay culture; one nurse
wants to come to a drag show with me. That’s good because a lot of straight people don’t
understand gay people. The other benefit is that the services understand gay men, so it’s my
chance to be with my kind of people, when I am with them I come alive. We can talk about old
times and I can be myself. Lizzi says there are more gay men like me with HIV who are going to
need aged care. Can you tell them my story so that they get looked after well and don’t get lonely
like me?
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
21
_____________________________________________________________________
Table 2: Précis from case study 2
Show a little fight girls, don’t be too polite.
Thelma, she was born in 1936 and was diagnosed with cancer in 2002 and died six months later.
We were together for 19 years. Thelma was, is and always will be the love of my life. She was a
wonderful woman and a very strong lesbian. She went in all the marches, spoke on the steps of
parliament house and chained herself to the arbitration buildings for equal pay for women.
Thelma was able to be cared for at home because of this wonderful chain of lesbians who stick
together and give support because we love each other and are committed to each other. The chain
also allowed me to survive after her death. If they weren’t around I think I would go mad. Caring
for Thelma at home was the greatest blessing for both of us. Every day was a new day for us. I
could see her nearly every second of the day. I could look at her, I could smile at her and I could
talk with her. I could spend my time with her and I had all the help I needed.
We had three close friends who were nurses that we trusted to care for Thelma. They were trusted
because they were friends and they were lesbians. They knew us both. We had a palliative care
service come in and the district nurse. When they came to see Thelma I said: “We are lesbians and
we would like to be recognised as a couple and we ask for your respect and I don’t want any male
nurses coming here to wash Thelma or whatever you people are going to do.” They agreed. The
case manager used to sit out the back and have a yarn with us. She knew we were lesbians. She
told me afterwards that she knew immediately she came in because there was this beautiful sense
of eyes looking at each other, the way I looked at Thelma, the way that Thelma looked at me. She
knew but she said that she appreciated me coming out to her. She would go to Thelma and kiss her
on the top of the head.
That was really nice. On Christmas day the palliative care nurse came
dressed as a rainbow fairy, which was amazing.
The palliative care service was there for advice, support and they were very much in the
background to let Thelma die the way she wanted to die with the people around her that she
wanted to have care for her. We were surprised at how supportive they were of us as a lesbian
community. They said to us that they had never come across this kind of support before. After
Thelma’s death, the case manager asked whether there anything else that they could have done for
us as a community. They used the word ‘community’ and ‘your community’.
The lesbian chain becomes more important as you get older. In your area there’s always a lesbian,
you know what I mean? There is always a lesbian for a little bit of a talk, a little bit of a smile, a
little bit of a joke. That is part of the wonderful chain of lesbians caring for and loving one
another. That is more important as you get older, it is very, very important. If older lesbians do not
have the support we had, and if they are not going to speak up then they are going to loose a
chance of having a wonderful life on their last years. If you don’t talk up you die very lonely. You
might have got some flack but who cares? You have to talk up, ask for help. If the worst comes to
the worst, well you are not a murderer, you are not a thief, you are just a very great lesbian who
loves women.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
22
_____________________________________________________________________
Table 3: Précis from case study 3
I am who I say I am
Nancy
: Me name is Nancy, I was born a boy in 1928 and me parents called me Brian. I worked as
a female impersonator with Les Girls and I went into the navy during the Second World War. In
1959 I had a sex change operation. I could only have the breasts done; they couldn’t do the change
below. I’m not a pure male any more; I’m a trans; both; fifty-fifty. Staff here know who I am.
Me life is hard. Its hard being in here. The people here are a lot of bludgers. I should keep away
from them. That’s why I never leave me room except for some meals. See! I’ve got me bags
packed. I’m leavin’. They’re not my kind of people, they’re not sociable people. One of the other
residents wants to flatten me because I’m a transsexual. Had I been a normal sex it would have
been a different story then. People judge me because I’ve got a penis, I’m a transsexual. If I didn’t
have the penis, if I was a full female, then it would be a different story. They wouldn’t know I was
a transsexual then. Sometimes I don’t want to funkin’ eat. Sometimes I feel like I wanna die. Me
life’s too fuckin’ hard.
Maggie
: When I first met Nancy my heart went out to her. To me Nancy was Nancy. Sometimes
she would pee standing up with the toilet door open and I would walk past and do a double take
and then go: ‘Oh! That’s right!’ Nancy dressed very inappropriately when I first met her. The staff
used to think it was funny when she walked out in a bikini with half her genitals falling out the
bottom of her bikini pants. They thought it was funny to watch her get around like that. When I
took over the place I fired the lot of them and helped Nancy to feminise herself. We were teaching
her how to be feminine and she blossomed.
Nancy was married to Frank for 18 years. When Frank was dying they took him to hospital.
Frank’s family told Nancy that she couldn’t visit him because it was ‘family only’. Well that was
the wrong thing to say to me, I said to Nancy: ‘You go upstairs, tidy yourself up, put a bit of lippy
on and get your coat; I’m going to take you to the hospital.’ Nancy stayed with Frank for about an
hour before he died, she was so happy.
I was at home the day after Frank died and the staff rang me to say that Frank’s nephew had just
arrived and was taking everything out of Frank and Nancy’s bedroom. They were trying to take
the rings off Nancy’s fingers. I reckon I must have broken all the speed rules to get there. I went
flying up the stairs and into the bedroom and I said to him: ‘Get out of here, before I ring the
police; how dare you! She hasn’t even had time to mourn and you’re trying to wipe out every
memory she’s got. Get out of the building before I call the police.’
Since Frank died Nancy has been lonely, she would talk to anybody and everybody. She is very
vulnerable, especially now. The staff here are so great, we are all very protective of her. I try to
teach my staff that what you see is what she is. Don’t think that’s Brian; that’s Nancy. That’s
Nancy through and through and to you she is a woman. If you get that through to them there’s no
dramas after that.
She is a woman
.
That’s how I have always treated her.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
23
_____________________________________________________________________
The components of GLBTI-friendly aged care services identified in
stage one
The report
My People
presented the experiences of 19 GLBTI seniors receiving aged care
services in Victoria. In the following section the implications of the research findings for
aged care services will be explored. The stage one study clarified that some GLBTI seniors
are exposed to discrimination in aged care services. The study also identified strategies to
address this issue. Firstly, participants expressed their support for GLBTI-specific aged care
services. Secondly, the need for education related to the needs of GLBTI seniors was also
identified. An exploration of these strategies follows.
GLBTI-specific aged care services
Most participants were supportive of GLBTI-specific residential aged care because of the
importance of being with ‘my people’. The support for GBLTI specific services was
articulated by Joseph. The staff working in such a facility,
would know what to expect. If it
offends them personally and professionally, then they would be smart enough not to offer
their services
(Joseph, 61 years, queer).
Educating aged care service providers
The need for the education of aged care service providers was explicitly described by some
participants. Perhaps the most pressing need for education relates to the legal responsibilities
of aged care service providers to provide non-discriminatory care. Other opportunities for the
education of aged care service providers were highlighted such as the phenomenon of ‘my
people’ and the associated service characteristics that enabled participants to feel cared for
and valued.
‘My people’
Most participants made explicit reference to the importance of ‘my people’. This referred to
family, friends and aged care service providers with whom they could be themselves.
Analysis of the conversations around ‘my people’ highlighted five key characteristics that
could be applied to aged care for the development of GLBTI-friendly aged care services.
These characteristics were understanding, empathy, trust, advocacy and leadership.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
24
_____________________________________________________________________
Understanding and empathy
Some participants thought that GLBTI service providers were better able to understand their
needs and empathise. Participants indicated that aged care service providers needed to
understand the needs of GLBTI seniors before they could feel safe to disclose their
sexual/gender identity. See Appendix 1 for some of the particular issues that arose related to
the need for staff understanding.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc
Permission to speak
25
_____________________________________________________________________
Trust
Most participants felt that they needed to trust their carers, particularly if they were
dependent on the aged care service provided. A sense of mistrust and fear was apparent in
many stories.
Advocacy
The majority of participants who reported positive experiences of aged care services had an
advocate. In some cases the advocate was a family member or friend; in other cases it was an
aged care service provider. Advocates generally understood GLBTI seniors, demonstrated
empathy, were trusted and played a pivotal role in crisis management ar ound incidents of
discrimination
Leadership
The need for strong leadership in policy and practice areas was also identified. Leadership is
based on the knowledge of existing legislation which prohibits discrimination on the grounds
of sexual/gender identity. However, the practical implementation of such legislative
requirements has fallen short in some aged care services.
The significance GLBTI seniors’ stories
The stories shared by GLBTI seniors in the stage one report provided evidence of
discrimination and a catalyst for change. The stories demonstrate the way in which
discrimination is perpetrated by staff, co-clients and visitors and by an aged care system that
does not acknowledge GLBTI seniors.
There remains the opportunity to create aged care services in which GLBTI seniors are given
permission to express their sexual or gender identity. Rather than giving lip service to the
notion, participants wanted to see service provider s demonstrate genuine commitment to
ensuring their safety and understanding of their needs.
These new understandings bridge some of the gaps in our knowledge of the experiences of
GLBTI seniors in aged care services and provide guideposts as to how to affect change. The
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
26
_____________________________________________________________________
findings from stage one provided a basis for service review and policy development at
government and provider level. Stage two of the Project involved focus group and one-to-one
interviews with aged care service providers.
Stage two: The perspectives of aged care service
providers
There is a common notion that older people are sexuality-less; they shouldn’ t be
having sex. That goes hand-in-hand with the dirty old man syndrome. Those two
things together: dirty and old. It is part of the capitalist notion that when we are
young we work and contribute to society and that once we retire we are
uselessness and go off and should not be seen or heard.
That is part of the social conscience, that older people should not be seen or
heard. If an older person is gay they stand out more and society says: How dare
you do this!
(Patrick; coordinator, GLBTI support and advocacy group).
Stage two of the program sought to explore the perspectives of aged care service providers
and determine strategies to create GLBTI-friendly aged care services. The project involved
two phases. The first phase included three focus groups with aged care service providers to
seek their feedback on the
My People
report and to determine strategies to create GLBTI-
friendly aged care services. The second phase involved telephone interviews with aged care
service providers who were unable to attend the focus groups.
Data collection
The primary method of data collection involved focus groups and phone interviews with aged
care service providers. Participants were sought thr ough the project steering committee
networks and direct contact with aged care service providers listed on the internet. Three
focus groups were conducted. The first involved carers in a privately run nursing home
(referred to here as ‘Hibiscus Heights’). Staff in the home initially made contact with the
project researcher to discuss the care of a gay resident.
The second focus group comprised team leaders in residential aged care services. The third
focus group consisted of representatives from community support agencies and advocacy
groups. Sixteen phone interviews were conducted with a range of aged care service providers
who were unable to attend focus groups.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
27
_____________________________________________________________________
All participants wer e provided with the executive summary of the
My People
report and an
information sheet and consent form. The participants were invited to respond to the report,
describe their experiences caring for GLBTI seniors and to identify strategies to create
GLBTI-friendly aged care services. Those participants who had not cared for GLBTI seniors
were invited to comment on the pr eparedness of their service to care for GLBTI seniors
described in the following vignettes adapted from the
My People
report:
1. A gay man with HIV/AIDS who is lonely and misses the gay community.
2. A lesbian feminist who has a loving partner and close circle of lesbian friends.
3. A transsexual woman who has a penis and forgets how to feminise her
appearance and behaviour.
4. A man who feels depressed and suicidal if he is not allowed to dress as a
woman.
Notes taken during focus groups and phone interviews were presented to participants for
verification and de-identification. Focus group two and three were also digitally recorded.
Characteristics of participating aged care service providers
The focus groups were attended by 20 aged care service providers. Focus group one,
consisting of participants from one private nursing home named here as Hibiscus Heights,
included: a care co-ordinator, a diversional therapist, a physiotherapy assistant, division two
nurses (2) and personal care attendants (3). Focus group two involved the director of nursing
and chief executive officer of a private nursing home (high care facility) and the director of
nursing for a private hostel (low care facility). The third focus group involved representatives
from nine community support agencies and advocacy groups which provided seniors’
services.
The phone interviews involved 16 aged care service providers including one chief executive
officer, director of nursing, geriatrician, academic, educator, division two nurse, personal care
attendant, two division one nurses and seven service managers/coordinators. The participants
worked predominately in the government sector (12) in Melbourne (12) and provided
services in residential aged care (3), home and community care (8), aged care assessment
service (1) and GLBTI support and advocacy (4).
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
28
_____________________________________________________________________
Table 5: Characteristics of aged care service providers participating in phone interviews
No Pseudon
Role Sector Service
ym
1 Alan Chief executive officer Government Hostel
2 Penny Division two nurse Private Nursing home
3 Hazel Division one nurse Government Nursing home
4 Jenny Educator Government Home & community care
5 Jean Academic; health professional Government GLBTI care & advocacy
6 James Health services manager Government GLBTI care & advocacy
7 Jack Division one nurse Government District nursing services
8 Vanessa Health service manager Government Home & community care
9 Penelope Director of nursing Private Nursing home
10 Lisa Team leader Government Home & community care
11 Patrick Community group co-ordinator Private GLBTI support & advocacy
12 Elizabeth Community group co-ordinator Private GLBTI support & advocacy
13 Denise Personal care attendant Government Home & community care
14 Marg Acting Manager Government Aged care assessment
Geriatrician
Hospital and community
15 Aviva
Government
care; education
Team leader- social worker
Home & community care
16 Angela
Government
To protect the identity of participants no further demographic details are provided. However,
it is interesting to note that some participants disclosed that they were gay or lesbian.
Certainly their sexual identity may have contributed to their awareness of issues for GLBTI
seniors and their willingness to participate in the project.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
29
_____________________________________________________________________
Findings: The context of aged care services
The key findings from the focus groups and interviews include description of the experiences
of aged care service providers and their suggestions for change. The experiences of aged care
service providers are described in this section. These experiences are drawn from a number of
themes relating to the context of care. These contextual factors, which need to be understood
and taken into account if change is to be successful, include:
1. Ageism, homo/transphobia and the broader community
2. Prudishness about sexuality in aged care
3. Cultural isolation for GLBTI seniors
4. The unknown needs of GLBTI seniors
5. The value of change champions
6. Gay men and fear of HIV/AIDS
7. People like that – fear of the unknown
1. Ageism, homo/transphobia and the broader community
Many participants reflected that ageism and homo/transphobia in the broader community
influences the aged care services provided to GLBTI seniors. It was generally agreed that the
community did not value seniors nor consider them to be sexual or sexually diverse. These
views were reported to be reflected in the care provided in aged care service services. Angela,
for instance, suggested that society was,
extremely discriminatory towards GLBTI people and
what happens in aged care is another symptom of that
.
(Angela, team leader, home and community care)
Elizabeth pointed out that older lesbians don’t want to face ageing, because of having to face
ageism & deal with how they will be confronted with society’s ageist treatment.
They fear
getting older and being disabled. … There is a fear of being old and a fear of elder abuse
behind the fear of being old. Women fear being vulnerable to abuse from their families, their
partner and aged care service providers.
(Elizabeth; coordinator, GLBTI support and
advocacy group)
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
30
_____________________________________________________________________
Others such as Patrick suggested that:
It is part of the capitalist notion that when we are young we work and contribute
to society and that once we retire we are uselessness and go off and should not be
seen or heard. That is part of the social conscience, that older people should not
be seen or heard. If an older person is gay they stand out more and society says:
How dare you do this!
(Patrick; coordinator, GLBTI support and advocacy group)
Ageism was also thought to exist within the GLBTI community with younger generations
feeling confronted by their own ageing. This lack of intergenerational support needs to be
challenged to ensure that the efforts of seniors’ advocacy and support services are valued. As
Elizabeth suggested, …
it can be difficult to attract younger lesbians. Younger lesbians want
older lesbians as role models but they wonder how much the issues for older lesbians are of
concern to them. They think that by the time they are our age we will have paved the way.
(Elizabeth; coordinator, GLBTI support and advocacy group).
The extent to which the creation of GLBTI-friendly aged care services needed to take into
consideration the community context was highlighted in relation to community care. Vanessa
described how a female home care provider was unable to provide home services to a lesbian
client because;
her husband would not allow it
. (Vanessa: manager, community care). As
indicated by Vanessa, aged care services providers are influenced by the homophobic views
of the community in which they live. The context of ageism and homophobia in the
community can also have a negative influence on the experiences of GLBTI seniors when
manifested through their families, other clients in shared services and when amplified in rural
communities.
Family control
Ageism and homo/transphobia, particularly from family members, had negative effects on
GLBTI seniors. Several participants shared stories of family members, who were
shocked if
their parents would do anything other than be old
(Focus Group 2: residential aged care
managers). Some family member s had sought to control sexual expression in dependent
relatives; some family members would not recognise the sexual or gender identity of their
family member or their choice of partner. This was highlighted by Vanessa who described a
lesbian grieving after the death of her partner of 28 years. The couple’s relationship was not
recognised by their families. Consequently, the devastated lesbian
had no input into the
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
31
_____________________________________________________________________
funeral; her partner’s family took over; she sat at the back.
Vanessa also highlighted that this
exclusion can come about because older rural lesbians are invisible.
In rural Victoria a lot of
lesbians are not out. Some of them have been living together for many years but haven’t
come out to work or to their family. So, when their partner
dies they are devastated because
they can’t tell anyone.
(Vanessa: manager, community care).
Heterosexual seniors
Homo/transphobic views were also reported to be held by heterosexual clients in shared
services. For example, in Hibiscus Heights several residents refused to be showered by a
male staff member who was openly gay. One hostel manager reported being approached by a
resident who had seen a television report on a lesbian marriage and said,
it’s disgusting and
you should see them; one of them looks like my father
(Focus Group 2: residential aged care
managers). While these responses were directed at staff they presented an obstacle to the
creation of GLBTI-friendly aged care services and meant that GLBTI seniors would,
need to
be very brave to disclose in aged care
(Focus Group 3: community support and advocacy
groups).
Sexual diversity and rural communities
Ageism and homo/transphobia were particularly apparent in rural areas. Aged care service
providers from these areas believed that rural communities were less aware of their GLBTI
seniors and less tolerant. Consequently, GLBTI seniors were more isolated and had fewer
opportunities to express their sexuality. Others suggested that in some rural communities
there are a
hell of a lot of people who are bigoted
because they don’t encounter sexual
diversity
(Lisa, team leader, home and community care). This presents a challenge for GLBTI
seniors who have community members coming into their homes to provide aged care services
and for those mourning the death of a same sex partner in a closeted relationship.
Issues related to people coming into the home are significant for GLBTI seniors who want
home support services. This is one of the most significant issues relayed to senior GLBTI
advocacy groups. As Vanessa stated,
for someone who is that closeted to have a carer come
into their home; they are in
dire straits in rural areas because they’re not out.
(Vanessa:
manager, community care).
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
32
_____________________________________________________________________
Jean also pointed out that
most GLBTI seniors receive aged care services in their own home.
It is difficult for
people in their own home if they have to de-gay their home because aged
care service
providers are coming in.
(Jean, lesbian, academic and health care professional)
Uncle Noel had services coming in from the start and they were not gay- friendly.
There were snide remarks made about being gay by the carers that were coming
in. He had gay stuff around in his house and the carers sniggered about that. But
by virtue of his strength he got what he demanded. Not everyone has that. Not
everyone is that assertive.
(Patrick; coordinator, GLBTI support and advocacy group).
The context of ageism and homo/transphobia in the broader community was an important
consideration in the development of GLBTI-friendly aged care services. It was argued that
the views of aged care service providers may not be any more discriminatory than those of
the general community. However, the dependency of GLBTI seniors on aged care services
meant that the negative ramifications could be greater. Furthermore, it was felt that ageism
meant that there were puritanical attitudes amongst aged care service providers.
2. Puritanical attitudes and sexual activity in aged care
Aged care service providers noted that many of their colleagues did not expect seniors to be
sexual. Carers were reportedly surprised if heterosexual couples were sexually active,
shocked if male client masturbated and appalled if female clients masturbated. It was
suggested that,
the whole aged care industry can’t get over the fact that any older person
would have sex
(Focus Group 3: community support and advocacy groups). It was also
postulated that because sexual expression and ageing were not expected to coexist issues
related to sexuality did not need to be addressed
As soon as you mention sexuality people think that you are talking about sex.
There is not enough distinction made between sex and intimacy. There is very
little discussion about intimacy and how we relate to a person in an intimate way.
I think that we have to be very car eful not to proscribe this in a narrow way.
(Focus Group 3: community support and advocacy groups)
Elizabeth also talked about the importance of clearly defining the relationship between
GLBTI issues and culture.
GLBTI activism is often seen to be only about sex rather than also
being about a range of issues related to our sexualities. GLBTI activism and sexualities are
defined as just about sex.
She also pointed out that repressive attitudes have silenced lesbians.
We need to be able to say this is what it is like to be a lesbian; this is what our sex
is like. … It has been taboo to speak about this for long enough. … We need to
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
33
_____________________________________________________________________
celebrate what we do and talk openly about our sex and female sexuality
generally
.
(Elizabeth; coordinator, GLBTI support and advocacy group).
Exploring the phenomenon of puritanical attitudes revealed numerous stories of service
providers who were frightened by residents who masturbated or too embarrassed to discuss a
rash in a resident’s groin or clean a resident’s penis. As Hazel noted, some of the staff are,
a
bit funny about residents having sex, a bit prudish, a bit sniggery, a bit conservative. They
don’t expect older people to have sex. It just doesn’t happen here
(Hazel: nurse, nursing
home). As sexual expression was not discussed many service providers were not prepared or
comfortable acknowledging seniors as sexual. Furthermore, as sexuality was often
understood as ‘sex’ and seniors were not considered to be sexually active, they were not
considered to be sexual.
Understanding sexuality and sex
Seniors were generally considered to be asexual. Consequently, sexual expression was not
acknowledged or welcomed. When sexual expression occurred the response was often an
intervention aimed at eradication. The meanings and stories for individual seniors were often
lost as Aviva noted:
Geriatricians are not good at acknowledging sexuality. There is increased
awareness when there are issues but it is addressed from a medical rather than
psycho-social perspective. Some geriatricians are positive about sexuality; others
struggle and are homophobic (Aviva: geriatrician, hospital/community care and
education).
At the base of a lot of homophobia is a fear of a different sexuality. There isn’t an
understanding of how a person can have a different sexuality, also that a woman
could be a lesbian but might also be straight for some of her life. Some women
deny their sexuality because they don’t want to deal with the oppression that they
might find.
(Elizabeth; coordinator, GLBTI support and advocacy group).
The indifference to sexualities can also be understood as indifference towards the cultural
isolation a GLBTI senior often experiences in aged care provision. Just as the concept of
sexuality was reduced to ‘sex’, being gay was often believed to be nothing more that the
choice of sexual partner. This happens in society generally, well before aged care provision
occurs.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
34
_____________________________________________________________________
The notion that seniors are considered to be asexual was highlighted at Hibiscus Heights
when a staff member reported that,
we have got a new resident; he used to be gay
(Focus
Group 1: Hibiscus Heights). The meaning of sexuality for gay seniors was debated by staff.
One focus group participant suggested that if Hibiscus Heights had several gay residents they
would need a ‘gay lounge’ so that residents could have sex. This was challenged by another
participant who argued that the residents,
might not even like each other; just because they’re
gay doesn’t mean they are going to want to have sex with each other
(Focus Group 1:
Hibiscus Heights). In that instance staff were willing to discuss their understanding of and
comfort with homosexuality and sexual expression. Participants in other services reported
that sexual expression was viewed as problematic and rarely discussed.
Problematic sexual behaviour
Regardless of sexual identity, residents’ sexual expression was generally considered to a
problem. As Aviva noted, s
exuality is an issue where there is aberrant behaviour, when
someone has dementia and there is sexual disinhibition, and it is raised as a management
issue
(Aviva: geriatrician, hospital/community care and education). The response of staff
involved eradicating sexual expression to relieve their discomfort and embarrassment. Unable
to articulate their discomfort staff provided an assortment of ‘irrational’ reasons why sexual
expression should be stamped out. One example involved a heterosexual couple who were
prevented from sharing a room by staff because staff,
were worried that if there was a
gastroenteritis out break the husband might pass it on to his wif
e (Focus Group 3: community
support and advocacy groups).
These responses promoted calls for aged care service provider to consider whether they,
put
their own values onto residents. We have to ask staff at what point they bring in their own
values. What about the resident? What matters to the resident?
(Focus Group 3: community
support and advocacy groups).
Aviva shared numerous stories of sexual expression being labelled as problematic or deviant.
In relation to ‘sexual disinhibition,’ Aviva considered that,
the staff’s initial reaction was to
assume it was a sexual problem and they would not tolerate anything sexual. Sexual
expression was viewed negatively and had to be stamped out. No-one tried to think of other
reasons
(Aviva: geriatrician, hospital/community care and education). Behaviours which
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
35
_____________________________________________________________________
appeared sexual were eradicated, rather than explored. Perhaps the most striking example of
this was the use of medication such as Androcur to suppress libido (Australian Prescription
Products Guide, 2008; Bayer, 2008; Queensland Corrective Services, 2006).
The suggestion that a libido suppressant needs to be a last resort was explored with the staff
at Hibiscus Heights. The nursing home contacted the researcher to discuss the needs of
Edward, a gay resident. Edward required nursing home care after his partner of 45 years died.
Suffering from dementia Edward believed that Phillip, another resident, was his partner.
Consequently, Edward would sit and hold Phillip’s hand and was once observed touching
Phillip’s thigh. This was discussed with Edwar d’s brother who informed staff that his brother
was gay. In the period after this Edward was prescribed Androcur and the staff contacted the
researcher to seek support in understanding Edwards’s needs.
Talking around sexuality and gender identity
Several aged care service providers noted that aspects of care that related to sexuality and
gender identity were considered,
not part of their lexicon
(Focus Group 2: residential aged
care managers). Conversations about this area were avoided because staff were
uncomfortable or unsure of a client’s sexual identity. Penny described talking ‘around’ the
sexuality of nursing home resident:
I looked after an old lesbian who would have been older than 70 and her partner
Beryl used to visit. We would talk with her around their relationship. We couldn’t
say the word lesbian because they never told us that they were. But we knew that
Beryl was the person who took home the clothes to wash and she was the one
who was recorded as the next of kin in the medical records (Penny: nurse, high
care).
Many participants reported that they ‘suspected’ that a client was gay or lesbian. Gay men
were generally considered to be more identifiable than women. The pattern of ‘talking
around sexuality’ created challenges for some carers who felt that more open dialogue could
improve client care. One such example was presented by Dana, who told of a colleague
assisting a male client to shower at home.
She has been caring for a gentleman who had quite large breasts. I remembered
(someone telling me of) a transsexual woman with a penis. This girl experienced
that. I asked her what she did and she said that she just kept her mouth shut. She
said that she just got taken aback. It opened her eyes and she just treated him like
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
36
_____________________________________________________________________
any other client. She didn’t say anything to him. I asked whether the council had
given her any information about him and she said that they hadn’ t. When we go to
someone for the first time they will give us a care plan or a ‘words up’ about a
client but they didn’t say anything to her. (Dana; personal care attendant in home
care)
Dana felt that if the carer had been briefed she may have been able to ease the client’s
embarrassment.
The silence around sexuality and ageing was considered to perpetuate the status quo. Some
managers felt that their staff required constant reassurance to say,
it is ok to talk about it
(Focus Group 2: residential aged care managers). Others clarified that, while it was ok to talk
about sexuality, it was inappropr iate to ask a client whether they were gay or lesbian because,
it is none of your business
(Lisa, team leader, home and community care).
Talking about sexual and gender identity amongst team members was considered a useful
means of creating a team that could support GLBTI seniors. Some aged care providers
readily identified and responded to these opportunities. Others were more reluctant to,
acknowledge what they know or see
(Focus Group 3: community support and advocacy
groups) or respond. Invisibility remained a significant barrier to education of staff. For
instance, Marg responded to the summary of the
My People
report in this way:
It was interesting reading but I don’t really know if we would do anything. We
don’t really have enough numbers of (GLBTI) clients to warrant education not up
to now. But things change all the time. We see about 5000 clients a year. With
everything else going on this would not be a priority unless we had the clients
(Marg, acting manager, aged care assessment service).
In other aged care services, participants noted that sexual and gender identity was not
discussed and discrimination often went unreported. In some services the only such
communication between staff was,
gossipy stuff; people would whisper and talk
(Penny,
nurse, high care) or,
laugh and snicker
(Hazel: nurse, high care) amongst themselves. Some
participants were concerned that this was also a symptom of an,
industry not well regulated
(Jack: nurse, district nursing services). However, it also seemed apparent that, without
education and dialogue, aged care service providers did not understand what it was that they
needed to do.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
37
_____________________________________________________________________
3. The unknown care needs of GLBTI seniors
Many aged care service providers were reported to believe that sexual identify was about sex.
Furthermore because seniors were expected to be asexual, being GLBTI was considered to be
inconsequential aspect of ageing. Consequently, there was a limited understanding of the
needs of GLBTI seniors. This “asexuality” was explored with the staff at Hibiscus Heights
who reported that the needs of their gay resident were no different from any other residents
because he was not sexually active. However, when the care needs of GLBTI seniors were
explored further, some staff reported that there was a need for,
awareness and sensitivity to
any discrimination from other residents or staff that may occur
(Focus Group 1: Hibiscus
Heights).
One could argue that unknown care needs means unmet care needs. This is a significant area
of concern. Whether a person’ s sexuality is a matter of privacy is a matter for debate. There
are many facets to the question of privacy and if sexual and gender identity are rendered
‘private’ then GLBTI seniors remain invisible.
I don’t believe clients should have to tell their carers that they are gay; it isn’t
anyone else’s business. I think that carers need to be given the information to
make them aware generally. There is an issue of privacy and confidentiality. I
would hate to think that in my later years that I would have to tell carers that I was
a lesbian. You would have female carers coming in and doing their top button up
because they would be
worried that I was staring at their breasts. It’s about privacy and courtesy.
(Dana;
personal care attendant in home care)
Understanding a person’s sexuality should really start before they enter the
service so that as they navigate the service system … at every step their needs are
understood and they will not slip the out of the net. We have to be careful that a
promised service is delivered. (Vanessa: manager, community care).
The third focus group consisting community support and advocacy groups gave this
question of privacy significant thought.
Care planning is geared for a particular purpose, around funding. The best we do
after the assessment is ask (the resident questions). … culture is paid lip service.
We have the Standards and Guidelines for Residential Aged Care Services and
there is a formula to follow. If you follow the formula and the Aged Care
Standards and Accreditation Agency comes in and if you meet that formula you
will be accredited. But if you scratch below the surface you realise that nothing is
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
38
_____________________________________________________________________
happening. (The cultural needs of residents are) …given lip service. The aged
care standards are good, (but the problem is) …how they are interpreted.
The staff (doing assessments and care planning) ask residents questions that fit in
with their idea of a good resident in a good facility. We need to ask residents the
question: What does that mean to you? (Focus group 3; community support and
advocacy groups).
Hiding the sexual and gender identity of GLBTI seniors from aged care staff and assessors
results in these seniors’ unmet needs remaining invisible.
In all the years that I have been doing this work I have not come across an older
person who was gay. We did have one person who made it known that he was gay
but he had to because he was HIV positive. … I can think of a couple of women
that we visited. They described themselves as really
good friends. They said that they used to work together and they lived together. I
just accepted that because I’m pretty stupid. I can think of a couple of older
school teachers, librarians and nurses who used to live together. There was
nothing to say that they were sexual but they may have been lesbians. (Marg,
acting manager, aged care assessment service).
The staff at Hibiscus Heights did not expect to care for a gay resident but sought support
from the researcher to meet his care needs. They had the courage to voice their discomfort
and seek strategies to improve Edward’s care. Their efforts highlight the opportunities to
create GLBTI-friendly aged care services through the education and resourcing of aged care
service providers. Having supportive staff provided the opportunity to assist GLBTI seniors
to manage the challenges of shared services such as residential aged care and day care
services.
4. The challenge of shared services
The limited privacy in residential aged care facilities presented particular challenges for
GLBTI seniors. Staff at Hibiscus Heights were aware of right of residents to privacy and the
responsibility not to infringe of the rights of other residents. Some staff noted that achieving
this balance meant compromises:
What you can do in your own bedroom at home is different.
You can run around in the nude at home. In here you have to quell that
( Focus Group 1:
Hibiscus Heights). The need to ‘quell’ sexual expression was one of the catalysts in the
prescription of a libido suppressant for Edward. Another was the perception that Edward’s
behaviour was predatory.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
39
_____________________________________________________________________
Well if it was a heterosexual or gay couple they would be okay if it was just a
peck or a hug. If they are doing a 10 minute snog then we have to tell them where
they can have some privacy. They’ve got the right to kiss, but they also have a
responsibility to the comfort of the other residents. The residents have the
responsibility to show tolerance. They are not living in their own home; they are
all living together (Focus Group 1: Hibiscus Heights).
A different situation was mentioned in the second focus group
One story that sticks out in my mind was this male resident that never told me he
was gay. He was a retired nurse and he never said that he was gay but you just
knew in a thousand little ways. He had a friend come in every day and he told me
that it was his nephew… It so wasn’t his nephew, it probably was his life partner.
..They couldn’t hug, he couldn’t stay the night and they had to pretend. I think
that it is very sad that this man is unable to have contact with his partner. (Focus
Group 2: residential aged care managers).
Other issues related to the challenge of shared services were also mentioned in focus groups
and included abuse from other residents and effect of lack of personal privacy on GLBTI
seniors.
Transgender people are between rock and hard place. We had a client who was
male to female who ended up in a facility for HIV positive women. The other
women there rejected her because they considered her to be a man so she was sent
to the male facility. The clients in the male facility considered her to be a woman
and rejected her. I am sure this kind of discrimination continues. Our members
pick on transgender clients. That’s another chapter. They are not large in number
but they have specific challenges and needs. We do have positive transgendered
people who are discriminated against. (James: health services manager, GLBTI
care/ advocacy).
I know of a gay couple who were both in low care. For some time they wanted to
have a commitment ceremony. One started to deteriorate and so his partner put
forward the ceremony. The staff were very supportive. One of them was
transferred to high care before the ceremony could take place. The staff in high
care said that they would not support the commitment ceremony. They were
worried about finances. They were looking for reasons not to support the
ceremony. They were worried about privacy and so on. Who owns the privacy? –
(Focus group 3: community support and advocacy groups).
One of the things that worries me with support is that we need to educate not just
staff but other residents who are homophobic as well. (GLBTI seniors) need to be
very brave to disclose in aged care. (Focus group 3: community support and
advocacy groups).
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
40
_____________________________________________________________________
5. The value of change champions
Most aged care service providers shared stories of GLBTI staff who championed change. It
was generally seen as role modelling. However, Vanessa coined the term “change
champions” in her interview.
We need care coordinators who can talk to their staff about these issues. We also
need champions who can work on behalf of particular clients. A champion might
just be someone from the community who can champion on the clients behalf.
Staff need to understand that there are different ways of doing things. They need
to provide a flexible service. (Vanessa: health services manager).
Having GLBTI staff was seen to bring,
awareness or normalness to being gay
:
we are here to
stay, its no big deal
(Penny: nurse, high care). Some organisations were reported to have,
just
enough staff there that it would have made a difference. They have an affect on staff. They
educate the other staff
(Focus Group 2: residential aged care managers).
Both focus groups 2 and 3 saw the importance of change champions. It was stressed in Focus
Group 3 that the champions need to be non-GLBTI as well as GLBTI.
When I worked as a manager in residential aged care staff knew that I was a
lesbian and all the gay and lesbian staff came out. … If I say I am lesbian it helps
people to come out. … I think (let’s) get some GLBTI older people out there to
provide education. … If you do have lesbian or gay men in (an) organisation
being the leaders it can easily come back against you. People can say that you are
only interested because it is about you. It is so important to have non-GLBTI
people involved in the change. … To get change we have to get a whole heap of
people as our allies. (Focus group 3: community support and advocacy groups).
Other stories of change champions involve aged care service providers who had exposure to
the GLBTI community in their personal lives. In Hibiscus Heights the staff who nominated
themselves as Edwards primary carers had family or friends who were gay or lesbian.
Consequently they felt,
more comfortable with caring for a gay man. We have had life
experience.e
(Focus Group 1: Hibiscus Heights).
Being comfortable caring for a gay man
enabled them to challenge the homophobic views of colleagues. For example, one of
Edward’s primary carers recalled how a colleague stated that homosexuality was ‘affronting’
and ‘repulsive.’ In response, the primary carer reported that,
I told her that my son is gay and
we have to accept that, so she has started to change the way she thinks.
(Focus Group 1:
Hibiscus Heights).
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
41
_____________________________________________________________________
Aged care service providers were positively influenced to understand GLBTI seniors when
they had a constructive relationship with a GLBTI person. These benefits were enhanced
further when the GLBTI person was a line manager. One example shared involved a lesbian
couple who were the director of nursing and chief executive officer of a nursing home. The
women were open with staff and residents about their relationship:
It is not unknown that we are a couple. We don’t hide it. ..We have started
modelling ourselves. We don’t set gay and lesbian aside as something different to
be tackled. .. Knowing the industry as well as we do, (we know) there is a
profound educational profile. It starts at the top in terms of management role
modelling. Staff learn from us that we are everywhere. They also learn that other
than the fact that we are in a same sex relationship, we do everything like the
others do. We are not standing up with pink strips, we are normal people. (Focus
Group 2: residential aged care managers).
Some cautioned that the reliance on change champions to create GLBTI-friendly services
could leave GLBTI seniors vulnerable if the champion left after the senior disclosed.
One of our gay r esidents chose our nursing home because I’m gay. … It worries
me that we have got no policies or procedures around sexuality and I am not
going to be there forever. I worry that he came under false pretences. What
happens when I leave? He thinks that he has come into a gay friendly nursing
home. (Focus Group 2: residential aged care managers).
Other change ‘champions’ involved entire team and organisations. For instance, the City of
Port Phillip and The Carlton Clinic were described as organisations that had a significant
number of GLBTI employees, understood the needs of GLBTI seniors and demonstrated
leadership in acceptance of diversity.
There is an opportunity to empower older people to empower themselves and
their families we have got gay workers. … I have been talking about cultural
diversity, it takes a long time to get other people to be your advocates, it just took
about 12 years to get people to understand it, it is far better for them to be saying
it than me. But the work on empowering older people and their families is great
(in the) interim… will change practice quickly. (Focus group 3: community
support and advocacy groups)
While many change champions were GLBTI or had contact with the GLBTI community,
others were simply motivated by empathy. The
My People
report documented the story of
Nancy, a transsexual woman and Maggie her carer who advocates for her across a range of
discriminatory encounters (pp. 73-80). Another powerful story of empathy was told by
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
42
_____________________________________________________________________
Penelope, a director of nursing caring for a cross dresser. The story is summarised in Table 7
(see following pages). The story encapsulates much of what was shared by GLBTI seniors
and aged care service providers including:
1. The enormous potential of aged care service providers to make a difference to
the lives of GLBTI seniors
2. The power of empathy and modelling respectful care
3. The importance of building trust in relationships with GLBTI seniors
4. The negative impacts of discrimination
5. The significance of history in planning care for GLBTI seniors
6. The impact of aged care service providers values and beliefs on care
7. The time and resourcing required for change
8. The need to provide permission for clients to speak about their sexuality
9. The need to provide staff with permission to discuss sexuality
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
43
_____________________________________________________________________
Table 6: One change champion’s story
It started with a smile:
Caring for a cross dresser in a nursing home
My name is Penelope. A couple of years ago I was the Director of Nursing (DON) of a high lev el care
facility. We had a gentleman, Dennis, who was in his mid seventies who had a stroke. Dennis was a
burly man who worked as a truck driver. When I took over the role as DON in that facility I heard staff
giggling about the fact that Den nis liked to dress in women’s clothing.
Having empathy and building trust
The staff used to ridicule Dennis because he liked to wear women’s clothing. I think that people fear
what they don’t understand. They don’t have to agree with what Dennis was doing but if they can
understand then they can support him. When I met Dennis I felt sorrow for him; I felt that this was him
as a person, a man who likes to wear women’s clothing. I felt sad that he could not be the person that he
was. I felt that if this is what he wanted to achieve then I would help him. I didn’t want him to have to
live a false life.
The staff used to catch him wearing women’s clothing and they found that quite funny. I struck a
rapport with Dennis and once I had his trust I asked him about dressing in women’s clothing. I
developed a rapport starting with a smile. He had difficulty speaking because of his stroke. After a
while he would be there at the front door waiting for me to arrive at work in the morning. When I
walked in he would always give me a high five. It grew from there. We would chat about general things
and after about 2-3 months we were talking about his life and he told me that he used to be married and
had a couple of young kids. When he mentioned that his marriage broke down I asked him was there
any particular reason why? He said no. Then I said: Do you like to dress in women’s clothing? He went
silent and a bit funny. I said that if he wanted to dress in women’s clothing he was able to. He said: No!
No! Then I said that if he wanted we could talk more and I would be there to help.
Culturally appropriate assessment and care planning
Days went on as normal and one day he came into my office and we had a big talk about it. Dennis told
be that it started when he was quite young. Every time he was found wearing women’s clothes there
were negative repercussions. When his mum found out she kicked him out of home. When his wife
found out their marriage fell apart and he was not allowed to see his children. When the staff found out
they laughed at him. When I first took over at the facility he just had small items like stockings. When
the staff admitted him they found stockings in his things. They thought it was funny. They were not
educated and didn’t understand.
Dennis was really embarrassed when I asked him about dressing in women’s clothing. I asked him if he
would like to wear the women’s clothing more often. I asked him what he liked to wear. He liked to
wear dresses and stocking s. He was reluctant to accept the offer of wearing the women’s clothing more
often. I said to
him that he could do that and the staff would not have to see. I invited him to have a
certain time of the day when he could wear the women’s clothing and I would make sure that no-one
went into his room; no-one could see him. He had private time between two and four o’clock in the
afternoons when he would get dressed. There were certain days that he wouldn’t do it. That was
because the staff that disappro ved were working. The facility was in a low socio economic area and the
staff could be a little rough around the edges. I think that there were some staff that when management
went home they could be inappropriate. You can’t be there all the time and unfortunately some staff
took advantage of that. Dennis told me that there were some lewd comments made to him by these
staff. He wouldn’t tell me what was said or who said it, he was worried about retribution. I asked him if
he wanted to be able to wear women’s clothing every day and outside his room. He said that he didn’t. I
think that he had had such a bad experience with the staff.
__________________________________________________________________________________© 2009
Matrix Guild Victoria Inc.
Permission to speak
44
_____________________________________________________________________
Table 6 continued
The other residents were not aware that he sometimes wore women’s clothing. He didn’t tell
them because he felt like he didn’t fit in with most of the other residents. We had some very
vocal residents who would have ridiculed him; we could not change their minds, being that
generation and cognitively impaired. He used to put the women’s dresses at the end of his
wardrobe so that the staff would not see them. It was easier to work with him than it was to work
with the staff. The staff were the most difficult, they did not see that it was about him as a
person.
Staff Education and cultural competence
The biggest thing that we needed was to try to educate the staff. Dennis needed assistance to get
dressed; he needed to have some staff on board. I got his permission to talk to staff. We ran a
session on the Standards and Guidelines for Residential Aged Care. If you run a session on
sexuality people won’t turn up. We started with a session on resident’s rights, then
confidentiality and then sexu ality. We ran sessions on sexuality over about six weeks. It was
such a big thing; we really opened up can of worms. We talked about the resident’s right to have
their life in the facility reflect their life at home as closely as possib le. We started with that, and
then we talked about sexuality in general. We talked about what would happen if a heterosexual
resident wanted a sexual relationship and their right to do that. Next, we broached the subject
about homosexuals and how the staff would feel if they were caring for someone who was
homosexual and wanted a sexual relationship. Some staff were horrified.
We had a gay staff member and that was great. He encouraged a lot of other staff to understand.
He was a driving force in that sense because at the education sessions he talked about what it
was like for him to be gay. He talked about his experiences and how difficult it was for him, then
he talked about how difficult it would be for a resident. After that one of the staff said: Do you
know that we have a resident who likes to dress in women’s clothes? I asked the staff how they
felt about that. Some of the staff said that it was wrong and that we should not even be
discussing it. I said that it was Dennis’ right to do this and this is his sexuality and this is who he
is. I told the staff that we are his advocates and we needed to help him. We discussed it openly
and I encouraged them to think about how Dennis would feel. I asked them to think about what it
would be like if it was you? That’s how we finished the session. Some of them wen t away and
did a lot of thinking and then came back with a slightly different attitude. This was over a period
of time, it took a while. Having such open discussion was a new thing and for the staff it was a
‘no-no’; they did not want to discuss sexuality; they just wanted to look at washing and dressing.
We had quite a large group of staff who were Christian Fundamentalists. They were horrified
and said that this was wrong. They were the minority, but I could never get them to accept who
he was. In the end most of them left.
After the education session I had two staff that were willing to accept and help Dennis. I told
Dennis, some of the staff are aware and would really like to help you. I asked Dennis to think
about whether he would like them to help him. He thought about it for a while and said that he
would give it a go. These staff provided him with the physical assistance to dress in women’s
clothing and did it without ridicule. Once Dennis was comfortable with these staff members he
began to allow them to help him. We started with two staff and then we had another one on
board, and then another. It took us nine months from the time I built a rapport with Dennis to the
time we got staff on board. It took him time to accept that staff wanted to help. It was Dennis’
first experience of being accepted wearing women’s clothing. I put in a big effort to educate staff
and I felt that for the first time he was with some people who accepted him for who he was.
Leadership
When I first met Dennis he only had small items of women’s clothing like gloves and stockings
and he was quite withdrawn and depressed. We took him shopping for dresses. He had make up
and he started to wear lippie outside the room as he got more confident and as we got more staff
on board. He was grateful to me, he would always say thank-you. When he was allowed to dress
as a woman it was like a huge weight had been lifted off him. He became more social and got
involved in groups. It made a difference to his mental health.
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
45
_____________________________________________________________________
6. Gay men and the fear of HIV/AIDS
The stories in the stage one
My People
report raised concerns with participants in stage
two about the level of education around HIV/AIDS. Participants were asked to
comment on the care of a gay man with HIV/AIDS. Penny’s reaction typified many of
the responses when she said that,
people would over-glove; there are always staff who
go too far; I don’t think staff have nursed enough HIV, so they would freak out
(Penny,
nurse, high care). Others like Hazel suggested that, s
ome staff might steer away
(from
this resident)
, not go near him, and avoid nursing him. They need the facts of how HIV
is transmitted and whether there going to be any dangers for them
(Hazel: nurse, high
care).
At Hibiscus Heights the staff reflected on Edward’s care thus: …
we don’t have the
information on whether he has AIDS. I feel sorry for the poor personal care attendants
that go in there and don’t wear gloves to protect themselves. If they get AIDS who are
they going to sue?
(Focus Group 1: Hibiscus Heights). While these fears have the
potential to damage Edward’s care they wer e easily eliminated through the provision of
staff education.
Gay seniors are aware of the stigma surrounding their sexual identity. James shared the
story of a 70 year old HIV positive gay man who was told that he required nursing
home placement. In response:
He decided that he didn’t want that; so he went off his antiretrovirals. He
chose death rather than go into a nursing home. Powerful isn’t it? He was a
very proud and independent man. Again issues of sexuality, ageing and
HIV/AIDS coming to an intersection. He chose death rather than go into a
nursing home (James: health services manager, GLBTI care/advocacy).
As people with HIV/AIDS live longer many more will require aged care services.
Consequently, to prevent discrimination education needs to be provided about the care
needs of people with HIV/AIDS. There were many references to education by
participants in the stage two study.
The training around sexuality should makes sure that people understand that
sexuality is only one part of a person’s life and does not represent the
person as a whole. Sexuality is one aspect, a large aspect and should be
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
46
_____________________________________________________________________
incorporated into culturally appropriate training that workers should get.
Not just sexuality, but a whole package. It all comes back to respect.
(Vanessa: health services manager).
This education also needs to explore the fears held by aged care service providers.
Focus Group 2 referred to education specifically in the area of HIV and that
consideration could also be given to establishing a residential care facility specifically
for people with HIV/AIDS.
I have had people come to me and they are really concerned because their
son is working with someone with HIV and they are really worried that they
are going to catch it. A lot of personal care attendants left school early in a
third world country so giving them education is going to be tough. As
people living with HIV… (are living longer it is now becoming a question
as to) …whether they look at opening a HIV specific facility. A lot of
people with HI V dementia are going to be hitting nursing homes. People
would do a lot better to have one here and one there, you might be able to
train your staff but you are always going to have your agency staff who are
going to refuse to wash them. (Focus Group 2: residential aged care
managers).
In such a facility staff could be educated around the need particular to the physical and
psycho-social needs of seniors with HIV/AIDS.
7. ‘People like that’ – fear of the unknown
Discriminatory views were particularly evident in the stage one report,
My People,
around the needs of transgender seniors. In considering a vignette on the care needs of a
transsexual woman from
My People
a number of stage two participants reported that
aged care service providers would not welcome her. Penny described how her
colleagues would:
… make a drama of it. There would be that talking at the desk; stuff that’s
really cruel. Staff would be passing judgements. You would hope that her
care would not suffer. The staff would not be outwardly cruel but they
would ignore her. If they decided that she was a woman, the whiskers
would be off, but the penis would throw them. She would be in the ‘too
hard’ basket. (Hazel: nurse, high care).
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
47
_____________________________________________________________________
Similarly Penny talked about how staff would be challenged because, in her small
town,
there just aren’t people like that
(Penny: nurse, high care).
I think people would be a little bit not quite sure how to cope with Nancy
(case study in stage one report,
My People
) in the beginning but I think,
especially if she’s got dementia, they would try to be a little more
understanding. The staff might be uncomfortable when they were showering
her because she’s got a penis, but they would get used to it. There just aren’t
people like that here. There are no transsexuals here. I think her shaving,
well there would be people who would laugh or snicker behind her back and
there would be people who would help her to shave. The other residents can
be very intolerant with each other. Some would alienate themselves from
her and others wouldn’t care. (Penny: nurse, high care).
Similarly, discriminatory responses were evident amongst clients in shared services, as
James suggested:
Transgender people are between a rock and a hard place. We had a client
who was male-to-female who ended up in a facility for HIV positive
women. The other women there rejected her because they considered her to
be a man so she was sent to the male facility. The clients in the male facility
considered her to be a woman and rejected her. Our members pick on
transgender clients (James: health services manager, GLBTI
care/advocacy).
Several participants expressed their concern that aged care service providers would
have difficulty meeting the needs of transgender seniors because they did not expect
clients to be transgender. In contrast, staff working in
residential services reportedly
expected that their clients were diverse and understood their care needs. Lisa suggested
that it was important to have conversations with staff about how they feel because,
people often look at
transsexuals and don’t take them seriously. We need staff
education so that we could
link them with the appropriate services.
(Lisa, team leader,
home and community care)
All my staff have worked with people with frail aged, intellectual
disabilities and mental illness and when you are with such a range of people
you have to learn to be flexible and respond to a range of needs.
(Lisa, team leader, home and community care).
These stories underscore the importance of context in considering strategies to create
GLBTI-friendly aged care services.
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
48
_____________________________________________________________________
The significance of context
The context in which aged care services are provided exerts influence upon the care
provided to GLBTI seniors. The themes highlight that the challenge of creating GLBTI-
friendly aged care services cannot simply be conceptualised as the interface between
heterosexist service providers and GLBTI seniors. Rather, the attitudes and beliefs of
aged care service providers are considered to be a microcosm of the ageist and
homo/transphobic views of the general community.
It could be argued that aged care service providers are no more enlightened than the rest
of the community. Seniors are not expected to be sexual or have diverse sexual and
gender identities and therefore aged care service providers have not received training in
this area. However, the community expects aged care service providers to understand
and respond to the needs of seniors who are dependent on them.
Perhaps the most pervasive factor in these discussions was the failure of aged care
service providers to discuss the sexual and gender identities of older people. In the
absence of accurate information being GLBTI was considered to be about ‘who you
had sex with’ and seniors were not expected to be having sex and therefore not
expected to be GLBTI. Consequently, management strategies, including libido
suppressants, were informed by a desire to stop sexual expression. Indeed,
conversations about sexual diversity and gender identity need to occur for change to
take place.
Aged care service providers have the opportunity to demonstrate leadership in the care
of GLBTI seniors and protect them from discrimination perpetrated by other service
providers, families, co-clients and the community. This was evident in the story told by
Penelope, the director of nursing who worked through numerous obstacles in her efforts
to support a male resident who wanted to cross dress (see table 7). In the following
section, the strategies identified by Penelope and other participants are explored.
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
49
_____________________________________________________________________
Strategies to create GLBTI-friendly aged care services
The previous sections of this report and the stage one report My People explored the
experiences of GLBTI seniors and aged care service providers to support the
development of GLBTI-friendly aged care services in Victoria. The following section
presents a summary of the strategies recommended by participants to create such
services. The strategies relate to eight core themes identified by aged care service
providers:
1 The importance of powerful allies
2 The immediate need for advocacy and support
3 The need to educate aged care service providers
4 The role of change champions
5 The opportunity to educate the community
6 The opportunity to empower GLBTI seniors and their advocates
7 The value of GLBTI-specific aged care services
8 The significance of research
9 The importance of legislation
Each of these themes is explored by presenting corroborating or disparate views of aged
care service providers. Next, from each theme strategies to create GBLTI-friendly aged
care services are identified.
1. The importance of powerful allies
Aged care service providers suggested that the scope and complexity of the change
required necessitated a coalition of allies to ensure its success. These allies need to
include those with the mandate to lead change, including the aged care industry and
government bodies. This high level support could enhance the strategic nature of
change processes and involve service providers who would not support change unless
they were given a directive to do so.
The importance of receiving support from government to translate evidence from
research such as that contained in the
My people
report and to make changes to policy
and practice was highlighted in the recent release of a mental health paper by the
Victorian Government Department of Human Services (2008). Several aged care
service providers noted that the paper, failed to address the evidence concerning mental
health issues in the GLBTI community.
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
50
_____________________________________________________________________
We need to think about awareness raising. I was surprised that the mental
health paper
(Because Mental Health Matters: A new focus for mental
health and wellbeing in
Victoria)
that has been developed by the Victorian
Department of Human Services has ignored the GBLTI community. All the
work that has been done around suicide and mental illness in the GLBTI
community that has been funded by DHS! We also have a gender dysphoria
clinic that is DHS funded. But the mental health paper has ignored the
knowledge and evidence around GLBTI people and mental health.
(Jean, lesbian, academic and health care professional).
The importance of powerful allies was also described by those GLBTI seniors reported
in the stage one report,
My People
, who were concerned that some aged care service
providers could ‘recite a mantra’ around acceptance of diversity whilst discriminating
against clients. There was general agreement that unless discrimination was monitored
and change was supported by government agencies, change would not be achieved.
There is not enough monitoring of practices. We are expected to produce
good outcomes but there are individual interpretations of what a good
outcome is. If you ask the right question you will get the right answer. As
auditors we see what we want to see.
(Focus group 3: community support and advocacy groups).
Aged care service providers recommended that a lobby group of powerful allies be
established to support the process of determination of strategies which arise from the
outcomes of this report.
Out of this we need a lobby group because they have a lot of power. A
lobby group would have the ability to enact change in government, in
funding bodies, Aged and Community Care Victoria, the ALSO
Foundation, Council on the Ageing, the National GLBTI Health Alliance,
Carers Victoria…
You’ve got the federal government who has got the HREOC (Human
Rights and Equal Opportunity Commission) Report which includes aged
care. Maybe it’s a good time to be raising awareness of GBLTI issues.
(Focus group 3: community support and advocacy groups)
Group members could also include Matrix Guild Victoria and Vintage Men. The lobby
group could assist in gathering the momentum for change. Certainly, the stories from
GLBTI seniors and service providers highlight the need for strategies to address the
immediate needs of those who are being discriminated against.
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
51
_____________________________________________________________________
2. The immediate need for advocacy and support
The immediate need for advocacy and support services for GLBTI seniors was
identified by aged care service providers and GLBTI seniors in
My People
. Both groups
expressed concern that strategies for change would not assist those who are already in
services where discrimination occurred. Furthermore, data from participants in stages
one and two revealed that those seniors who had positive experiences of aged care
services and those who were able to negotiate positive outcomes in response to
discrimination were those who had advocates.
Collaboration between existing advocacy and support services would assist with the
need to educate those within the aged care industry around the needs of GLBTI seniors.
This could provide some avenues towards immediate resolution for those currently
experiencing discrimination in aged care services. Advocacy and support groups which
could be involved include: Seniors Rights Victoria; The Community Visitors Program;
The Aged Care Standards and Accreditation Agency; Matrix Guild Victoria; Vintage
Men; and The ALSO Foundation. (see resource list at attachment 2). Engaging with
these groups about the historical experiences of GLBTI seniors and their existing care
needs could support their services to meet the needs of GLBTI seniors. This could
provide pivotal support for GLBTI seniors receiving aged care services while a broader
program of education is developed and implemented.
Indeed, one of the participants suggested that GLBTI support and advocacy groups
need a higher profile.
At a larger picture level it is necessary for older lesbians to know about
community organisations that can provide them with support and
knowledge of their rights. They need to have knowledge about where they
can turn for personal, cultural and legal support.
(Elizabeth; coordinator, GLBTI support and advocacy group).
Another participant suggested a simple strategic approach through which organisations
could be better linked: that there be created a
list of organisations that people can
access
, which could be made available across the sector.
(Vanessa: health services manager).
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
52
_____________________________________________________________________
3 The need to educate aged care service providers
Participants across both stages of the program highlighted the importance of education
in creating GLBTI-friendly aged care services. Concern was expressed that sexual and
gender diversity education is not currently part of training for aged care service
providers because sexuality was not considered to be important to seniors. The
provision of education that includes information about a diversity of sexualities and
gender identities, as well as issues relating to GLBTI cultures and ageing could provide
the opportunity to impart new knowledge and skills, challenge homo/transphobic values
and beliefs and give staff permission to speak about sexual and gender identity.
Several participants expressed concern about the lack of training accessed by aged care
service providers. Patrick commented that aged care service providers could be,
driving
trucks one day and caring for people the next
(Patrick; coordinator, GLBTI support and
advocacy group). Others suggested that,
the more education you have the more likely
you are to see your own homophobia and try to correct it; at least in a work situation
(Angela, team leader, home and community care). Education was required to ensure
that staff understood what was required of them. However, as Jean and others
articulated, it was
a cop out (for service providers) to say that they didn’t understand,
given there is a diversity framework in the Department of Human Services that
highlights the importance of culture. We need to make that link for GLBTI service
providers
(Jean: academic, health professional, GLBTI care/advocacy). For service
providers, making that link involves understanding legislative requirements and coming
to recognise sexual and gender diversity as culture.
Many participants mentioned training alongside the need for education of service
providers, as comments from one focus group demonstrate:
Education needs to be targeted to senior management because they are the
ones that drive change or not. They need someone to tell them about
professional responsibility to say what is ok and it is ok to be different. We
need people who model at a management level. We need little stories which
give us hypothetical(s). We need to start chipping away at the edges. We
tell stories. The majority of people that are not educated don’t learn with
words they learn with hypotheticals.
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
53
_____________________________________________________________________
We need compulsory education because it is always going to be a handful
of people who will take it up. They need to be educated about the
legislation.
Need education for tertiary institutes and to create the opportunity to talk.
(There could be) set up replays and scenarios and workshops to confront
people.
(Focus Group 2: residential aged care managers).
Conceptualising sexuality and sexual and gender diversity as culture
A number of GLBTI seniors in the stage one study
articulated that aged care service
providers did not understand what gay was. This proposition was evidenced in their
own stories and the focus group and interview data from aged care service providers.
Being GLBTI was often conceptualised as ‘who you had sex with’ and people in same
sex relationships were considered by some to be,
sexual deviants
(Angela, team leader,
home and community care). Others agreed that it was necessary to define sexuality
because,
as soon as you mention sexuality people think that you are talking about sex;
there is very little discussion about intimacy and how we relate to a person in an
intimate way
(Focus Group 3: community support and advocacy groups). The need to
focus broadly on sexuality and sexual and gender identity as culture was also
emphasised by Jean who suggested that:
It is a classic error to label GLBTI seniors by their behaviour only. They
have multiple identities and different cultural perspectives. We all have to
exist to some extent in the heteronormative culture. For GLBTI seniors who
have lived most of their lives closeted, the majority of their culture is
heterosexual but a part of them is gay. This is an innate part of people that
is important to them and when they have to suppress it they can feel
silenced and not truly themselves. Health professionals need to see GLBTI
issues as about cultures, which is what the
My People
report is about,
different social networks, belief systems and values. This group, whether
closeted or not, at least part of their culture is GLBTI. It is not just about
their behaviour, most are not behaving in a gay way.
(Jean: academic, health professional, GLBTI care/advocacy).
The concept of culture is familiar to aged care service providers. However, frameworks
for cultural competency are often interpreted as relating to ethnicity.
The education that is currently provided around discrimination is more
focused on culturally and linguistically diverse (CALD) than sexuality. That
hasn’t happened with us as a culture.
(Angela: team Leader, social worker).
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
54
_____________________________________________________________________
We need culturally appropriate services. We have culturally appropriate
services for CALD people but not for GLBTI people. We don’t know what
being GLBTI means for aged care. We don’t even have language for it. We
talk about GBLTI friendly aged care but we don’t know what that means.
(Vanessa: health services manager).
Culture is paid lip service. .. If you follow the formula and the Aged Care
Standards and Accreditation Agency comes in and if you meet that formula
you will be accredited. … Some people think that meeting cultural needs is
having a culture care kit on their shelf. ( Focus group 3: community support
and advocacy groups)
Vanessa clearly explained how this problem can be addressed for the recipient of aged
care services.
Education needs to start with those who are doing the assessment of the
older person’s needs. .. If there is an issue missed, if they don’t identify it
then the client is not tapped into the supports, the mentoring and they miss
an important level of service. Their needs have to be identified at the level
of the Aged Care Assessment Service. … I know lots of people that would
not disclose. It’s the way that it is asked. You don’t ask straight out: Are
you GLBTI? You say to a person: The reason that I am asking is because
we would like to see you receiving the services that you require. I would
like your permission to give this information to the people who are caring
for you. You need to do this so that they don’t have to tell people
themselves when they front up to the service. The next step is the full on
assessment. This is done in their own home, before they get services.
(Vanessa: health services manager)
This issue was also aptly pointed out by Jenny, an educator teaching aged care workers
using the ‘Community Services Training Package: Working effectively with culturally
diverse clients and co-workers’ (Community Service and Health Industry Skills
Council, 2002). This package articulates that students must
be made aware of
culture as
a factor in all human behaviour
(and have) respect for cultural diversity (including)
work practices (which) may relate to persons of diverse sexual preference
(p.641).
However, Jenny’s efforts to include GLBTI seniors in student learning were dismissed
by her managers as inappropriate
.
Jenny lamented that the impact on students was that
they graduated,
believing that sexual orientation is not a legitimate, or relevant or valid
subject and has no bearing on anything except what people do in their bedroom. It’s
very dismissive
(Jenny: educator, community care).
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
55
_____________________________________________________________________
Many stage two participants were interested in addressing the problems they have
experienced with the lack of a conceptualisation of sexual and gender identity as
culture.
Education needs to come back to culture. Can aged care service providers
be educated to think of sexuality as culture, not just what people do or don’t
do? There are communities built around it. I think it is a cop out not
understanding it well enough. Given there is a diversity framework in DHS
that highlights the importance of culture we need to make that link for
GLBTI service providers. Sometimes the different parts of the system don’t
talk to each other very well. (Jean: academic health professional).
While conceptualising sexuality as culture was intended to enable a broad definition,
some aged care service providers suggested definitions that were broader still. In
particular, suggestion was made that,
there is complexity around what we have to deal
with; there are a range of permutations of GBLTI. I really think that we need to deal
with is individuality
(Focus Group 3: community support and advocacy groups).
Our members pick on transgender clients. … They are not large in number
but they have specific challenges and needs. We do have positive
transgendered people who are discriminated against. There is a bit of a
pecking order (with) HIV. It is one thing to have HIV/AIDS but if you have
Hepatitis C you don’t own up to it. The clients are more fearful of finding
out that they are Hepatitis C positive because they are generally regarded as
injecting drug users and have a lower social status. Assumptions are made.
They are a marginalised group within a marginalised group. (James: health
services manager).
It is a classic error to label GLBTI seniors by their behaviour only. They
have multiple identities, different identities and different cultural
perspectives. We all have to exist to some extent in the heteronormative
culture. (Jean: academic health professional)
Aged care is so mono-cultural or one minded. Diversity is not considered
the norm. There is the bigger picture that everything is geared to a mono-
cultural world. There is a mantra around the need to treat everyone the
same ( Focus group 3: community support and advocacy groups)
People think that GLBTI community is homogenous but it is not. What we
need is respect for culture. We don’t have that sense of respect for
people’s culture. It is not about empathy; it’s not about tolerance; it’s
about respect. (Vanessa: health services manager)
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
56
_____________________________________________________________________
In addition to these suggestions for the content of education provided to aged care
service providers, a number of suggestions were made about the delivery of education.
We need education. We need to per severe with educating people…If
people are going to discriminate and are going to be honest about it, if
they had the balls to come out and talk about being a homophobe ,they can
be given fur ther education. We could have a gay bloke talking to them
about their experiences and they can develop a feel for what it is like for a
gay person…We need to ask carers for anonymous feedback or ask them
one-on-one about what they want about these issues. We need education
provided by someone with qualifications in the area, rather than the
straight team leader.
(Interview)
Methods for delivering staff education need to take into account relevant factors such as
the high turnover of staff, low literacy, limited exposure to GLBTI seniors and the
impact of individual providers’ values and beliefs on the care that they provide.
Suggestions for accommodating these needs included: stories that captured the voices
of GLBTI seniors; workshops with experiential and interactive learning activities; and
practical strategies for care. Systems for education were considered important and
could include staff orientation programs and other mandatory training. These processes
of education were considered to give staff permission to speak about GLBTI seniors.
Participants reported that these processes were accelerated by the presence of change
champions. Education by GLBTI seniors themselves could also prove to be an
important model.
4. The role of change champions
In many of the stories shared by GLBTI seniors and aged care service providers
mention was made of positive outcomes being achieved by change champions. In many
cases the champion was a GLBTI aged care service provider.
I think that there is probably a lot less homophobia where I work because
everyone knows that I am gay. (Focus group 2).
When I worked as a manager in residential aged care staff knew that I was
a lesbian and all the gay and lesbian staff came out. I was the talk for a
long time. Even personally it’s all about education and I would put it [my
sexuality] in their face. I got people on board. If I say I am lesbian it helps
people to come out. (Focus group 3).
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
57
_____________________________________________________________________
GLBTI staff often raised awareness in colleagues of the normalcy of being GLBTI and
provided support for colleagues to understand the challenges a GLBTI senior might
encounter. Others were actively involved in advocating for the rights of clients.
I think that the main issue is cultural isolation. On an immediate level our
organisation is involved in advocacy and lobbying governments for
changes to policy and services. On an everyday level working with seniors
the main thing that we confront is cultural isolation. (Interview Elizabeth).
The opportunities for improving care through the provision of GLBTI staff were noted
by Aviva who suggested,
I would like to see enough gay workers to create gay friendly
aged care. We are not going to be able to convert workers into sympathetic people
overnight
(Aviva: geriatrician, hospital/community care and education).
Champions of change were not only GLBTI carers. There are a number of stories that
described the powerful advocacy work of heterosexual carers. These champions
included Maggie (see table 4), Penelope (see table 7), and the staff from Hibiscus
Heights. These women shared a willingness to learn about the needs of their GLBTI
clients.
There is also a need for senior GLBTI support and advocacy groups to
have a higher profile. We need support from government so that we can
have a higher profile in society, and so that we can monitor abuse and
offer alternatives to heterosexuality. (Interview Elizabeth).
Such change could provide immediate improvements in the care of GLBTI seniors
while more long term strategies, such as education across the whole aged care sector,
the provision of broad based formal advocacy to GLBTI seniors and the development
of GLBTI-specific aged care facilities, take effect. However, supporting change
champions is not a substitute for systemic change. This was emphasised by a service
manager who described a gay resident choosing his facility after recognising that the
manager was gay. While this meant that the resident was well looked after, the manager
was concerned that if he left, the organisation had no policies on sexuality, and the
resident could find himself out in a homophobic facility. He commented:
It worries me
that we have got no policies or procedures
around sexuality and I am not going to be
there forever. I worry that he came under false pretences. What happens when I leave?
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
58
_____________________________________________________________________
He thinks that he has come into a gay friendly nursing home
(Focus Group 2:
residential aged care managers).
While the opportunity to support change champions is certainly one way to move
forward, it does not replace the need for change in other areas such as generic education
of aged care service providers and the community generally.
5. The opportunity to educate the community
A number of aged care service providers identified that their colleagues were a
microcosm
of the general community and reflected the homo/transphobic views of the
general community. Consequently, it was felt,
until society says that we are not going
to tolerate homophobia, it won’t change…
It will only change by the gay community
being strong enough to get society’s support; like we have done with gay marriage
.
(Patrick; coor dinator, GLBTI suppor t and advocacy group).
One stark example of the need for community education was the home carer whose
husband banned her from visiting the home of a lesbian client to provide care. This
situation highlighted the need to see discrimination in aged care services in the context
of community perceptions.
It was beyond the scope of this research to seek suggestions regarding ways to
accomplish the significant task of educating the community. The enormity of the task
was highlighted by Patrick who cautioned,
we are kidding ourselves if we think that we
can do a few reports and think that everything will change
(Patrick; coordinator,
GLBTI suppor t and advocacy group). While there is no suggestion that this report will
prompt significant change, there is some evidence that the project itself has already
raised community awareness and garnered a significant level of media interest (see
media interest register, attachment 2).
6. The opportunity to empower GLBTI seniors and their
advocates
A small number of stories shared by GLBTI seniors in the report from stage one
My
People
described the capacity of empowered individuals to ensure that their care needs
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
59
_____________________________________________________________________
were met. Some aged care service providers expressed concern that such stories should
not be held as an example for others regarding the means by which they could assert
their own needs. Particular concern was expressed that individuals have differing
experiences and responses and could not be expected to replicate the techniques used
by others. However, there was a general consensus amongst aged care service providers
that the opportunity existed to provide information and resources for GLBTI seniors
and their family, thereby assisting GLBTI seniors to advocate for themselves. That
particular residents were able to act in an empowered manner is indicative that once
empowered, GLBTI seniors could become aware of and successfully claim their rights.
.. there was an openly gay, very assertive, lesbian woman; she was the
type of person no one would dare mess with. I used to bring in the gay
press for her each week. She was the type of person that no one would
mess with: ‘I am out and proud - deal with it. ( focus group 2).
However, this needs to be countered by the fact that some residents such as those with
dementia will require formal advocacy support so that they are not ostracised.
We had a female resident and some of the staff were not comfortable
caring for her. She used to touch the staff on the breast, so they were
worried that she was a lesbian. She had been married but that doesn’t
mean anything. She might have just been mucking around but some of the
staff were worried that she was a lesbian. She used to grab staff on the
breast and thighs and she used to do this thing with her tongue like an oral
sex gesture. Maybe she was a lesbian and because she had dementia she
didn’t realise what she was doing. People used to talk about it and wrote
about it in her notes. (Hibiscus focus group).
Empowerment was viewed as a useful strategy for all GLBTI seniors, with specific
relevance for older lesbians. These women were thought to be particularly vulnerable
and in need of educational support. Elizabeth suggested:
There is a need to educate our community. We have to encourage (older
lesbians) that are over forty years of age to recognise that they are getting
older and that this is natural part of life. It is not an easy thing to do. They
fear getting older and being disabled. The fear is quite ingrained and deeply
felt. They fear being vulnerable because of physical incapacity. The fear of
death is deeper behind that. They fear their physicality. They fear
dependence on other people. There is a fear of being old and a fear of elder
abuse behind the fear of being old. Women fear being vulnerable to abuse
from their families, their partner and aged care service providers. And
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
60
_____________________________________________________________________
cultural isolation makes them feel vulnerable. (Elizabeth; coordinator,
GLBTI support and advocacy group).
Elizabeth also shared stories of older lesbians in heterosexual marriages that they were
unable to ‘leave’ until their husband died. Information and assistance could be offered
to these woman and other GLBTI seniors to enable them to understand their choices
and seek support. Such information, it was suggested,
could also be provided to
families and friends who may also be positioned to support GLBTI seniors.
It takes a long time to get staff on board to be your advocates. It has taken
me 12 years to get people to understand the importance of cultural
diversity. It is far better to have staff working in aged care services
advocating for cultural diversity that to have me saying it. It takes a long
time, but empowering older people and their families is a great interim
strategy that will change practice quickly. (Focus group 3).
It was acknowledged that not all aged care service providers would welcome the idea of
providing services to empower GLBTI seniors. Penny described how,
nurses hate
patients who take control, they like to be in control. If you said ‘feminist’ they would all
roll their eyes into their head. They prefer if you are vulnerable and pathetic
(Penny:
nurse, high care). Many agreed that changing practice takes time, however,
empowering
older people and their families is great interim strategy that will change practice
quickly
(Focus Group 3: community suppor t and advocacy groups).
Empowerment of GLBTI staff was also raised as a significant strategy for creating
positive change.
There is an opportunity to empower older people to empower themselves
and their families. We have got gay workers We need to support older
people and GLBTI staff. (Focus group 3) .
Myself there are lot of clients that I wouldn’t out myself to. The home care
office knows that I am a lesbian. I wouldn’t tell a lot of clients because if I
did they would say that they do not want me back. How about some
research in that area? What about the challenges for us? We need to see
whether there are backwards prejudices. We need people to accept us
regardless of our sexuality. I would be concerned about not getting work if
I told a homophobic client that I was a lesbian. I do feel that there is a part
of me that I have to hide. When I go to a new client they always ask: Are
you mar ried? What did you do on the weekend? I would like to speak
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
61
_____________________________________________________________________
more openly about what I do. I would like to tell them about my girlfriend.
It’s not that I have a need to share, but I wish I could do that a little bit
more without fearing that I could upset someone. (Interview Dana).
We have got a staff member who has a lot of contact with the community.
She doesn’t try to hide her sexuality or who she is, for most people it
would be clear that she is a lesbian. I have never had a staff member who
is so loved by the community. At Christmas our office was full of gifts for
her and most people would know that she was a lesbian. She doesn’t have
lesbian tattooed on her forehead but she has a stereotypical look. She
doesn’t wear makeup and high heels, neither do a lot of the other staff, but
she is clearly a lesbian and she is definitely adored. (Interview Lisa)
7. The value of GLBTI-specific aged care services
Most GLBTI seniors who participated in stage one of the project discussed the notion
of GLBTI specific services with much enthusiasm, believing that such services would
enable them to be themselves.
Aged care service providers were more cautious about
this option. They expressed concerns about how such services would be staffed and
whether they would receive support from the government and aged care service
providers.
One of the gay residents at work - I am the only person that he has come out to.
He meets his boyfriend outside the facility. He would make a beeline for a gay
facility…he would do really well in a gay facility. It is so sad to see someone
not able to hold their head up. (Focus group 2).
As people are living with HIV longer there is the question of whether they
look at opening a HIV specific facility. A lot of people with HIV dementia
are going to be hitting nursing homes. People would do a lot better to have
one here and one there you might be able to train your staff but you are
always going to have your agency staff who ar e going to refuse to wash
them. You could have a gay orientated rather than specific facility. (Focus
Group 2).
I think a there would be a difference in a gay and lesbian facility. They
could focus in a different way than a larger generic facility could focus.
My idealistic assumption is that there would be a high sense of ownership
by the residents, a feeling of safety and security and acceptance. The other
side of that coin is you got to have the staff; that is where I would
anticipate a very great problem. What happens behind closed doors… you
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
62
_____________________________________________________________________
are not always there to monitor what is happening, what they are actually
saying. (Focus group 2).
However, others such as James did not see staffing as a potential problem.
We need a purpose built home for people who are gay to end some of
these discriminatory practices. There would be so many gay and lesbian
nurses who would staff it. (Interview James).
The development of GLBTI-specific options was not seen to ameliorate the need for
education and standards across the mainstream aged care sector.
I still believe that there is a need for a gay and lesbian facility but that does
not mean that the overall standards and tolerance level…(are not) raised
and addressed across the entire industr y. I don’t think that one minority is
so specific from another minority that generic education can’t raise it to a
level where all minorities are respected. Not just tolerated but respected.
(Focus group 2).
However, aged care service providers acknowledged that, given the challenges for
GLBTI seniors in existing aged care services, the enthusiasm for specific services was
hardly surprising. A number of aged care service providers suggested that there was a
need for more research around what GLBTI seniors wanted from these services.
I would like to see a survey that is broad based. We need to ask if people
want a gay and lesbian facility or whether we are just kidding ourselves in
terms of what we want to see. Does the community really want it? Do we
really need it? Most people don’t think about it and then they are
desperate. We need to find out exactly what it is that they need and then
we can ask the department for it. The qualitative work that you have done
is very important. Governments want quantitative data. We want it, we to
see it also. We want to see something in the area but we don’t know what
to do. We need more factual information.
I am not convinced. I still would love to. It has been our dream but I am
not convinced.
I think it would be awful to work in a GBLTI facility, they would be really
demanding.
What service is it that this community actually needs? It hasn’t been
articulated.
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
63
_____________________________________________________________________
In terms of aged care, there has been talk but I am not hearing convincing
answers why there is something needed for the gay and lesbian
community.
(Focus Group 2).
8. The significance of research
The research reported here aimed to explore the experiences of aged care service
providers in order to determine strategies to create GLBTI-friendly aged care services
in Victoria. This report and the
My People
Report presented evidence that GLBTI
seniors have special needs and are discriminated against in aged care services. As such
these reports provide evidence that contributes to a momentum for change.
Certainly this research could be replicated across Australia. Further research could also
be undertaken to explore the experiences of intersex seniors, GLBTI seniors in rural
areas, homo/transphobic staff and their responses to GLBTI seniors. Further research
could also explore the strengths and coping strategies of GLBTI seniors and evaluate
interventions for change.
You can set up supports but whether a person takes them on or not is a
different matter. For example you can have a GLBTI friendly facility and
women still don’t come. This is the more subversive work that we need to
do; we need to change the attitudes of older lesbians as well as people in
general, on that deeper individual level. We need more research and we
need theoretical analysis of data to achieve this deeper level of change. On
that really deep level there could be mor e subversive work done with
wider policy ramifications. And of course as well there has to be
campaigns and reforms on different levels.
I think that we need to do more research too on what younger lesbians
want and on ageism in the GBLTI community. Often younger dykes say
that they are not interested in coming to events involving older lesbians.
This is a form of ageism. It doesn’t appeal to them and they exper ience a
feeling of vulnerability when they are confronted with their own ageing.
Women say that the most difficult thing that they have to confront is their
old age. People don’t want to know and unless we confront them with
lesbian issues that are involved with the ageing process then a group for
senior GLBTI support and advocacy is just a voice crying in the
wilderness.(Interview Elizabeth).
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
64
_____________________________________________________________________
9. The significance of legislation
Most aged care service providers articulated the importance of providing education in
relation to the legislation developed to protect GLBTI people from discrimination. An
awareness of the legislation would reportedly,
go a long way to making a difference
(Focus Group 2: residential aged care managers). Others agreed that,
even though I
can’t change some of staff values, I can make them aware of the legislation
(Alan: chief
executive officer, low care). Some participants thought that aged care service providers
don’t understand how discrimination manifests in practice
. (Focus Group 2: residential
aged car e managers). Therefore, an understanding of the legislation could change
practice by highlighting the responsibilities of aged care service providers to protect
GLBTI seniors from discrimination. This ‘bottom line’ approach pr ovides the
foundation to conceptualise sexual and gender identity as culture.
The basic education for the personal care attendants means that they all
know that they can’t discriminate against a Muslim or a black person.
Still, I get people say outrageously homophobic things to me about gay
residents even though they know that I am openly gay. They just don’t
understand. They have no idea that there is legislation against what they
are saying. No idea; they are totally oblivious to how inappropriate it is.
(Focus group 2).
We need to report people who breach the law…we need to write
incident reports when discrimination occurs. (Focus Group 3).
The biggest change to make improvements for residents is to clarify the
regulations. We need good industry standards of care. We need to be
proactive. (Interview Ray).
The whole issue needs to be hit really har d. We can’t continue to skirt
around the edges. We can take it right back to the law and say that it is
illegal to discriminate against someone because of their sexuality and
put it out there that it is illegal. We need to say: Do you know it is illegal
to discriminate against someone because of their sexual identity? If you
are not meeting the standards I am going to report you. We have to hit
their achilles heel. We need to tell them that their funding is tied to the
standards and if they discriminate we will report them. They will loose
their funding. I am sick of skirting around the edges. It has gone on too
long. I am a registered nurse and I do agency in lots and lots of places
and I work at the director of nursing level. I am empowered to use the
system and I know the chain of command and who to report to. Some
people find that threatening and I don’t care. If they are not meeting the
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
65
_____________________________________________________________________
standards if they are not meeting the law I report them. I fill out an
incident report and they have to address it. (Focus Group 3)
Conclusions regarding strategies for change
The strategies presented in this section represent feedback from aged care service
providers. Participants in the stage one research also recommended similar strategies
for change with differing emphasis. For example GLBTI seniors emphasised the
importance of personal history or prejudice and persecution and the positive prospect of
GLBTI-specific aged care services.
In the report My People, GLBTI seniors described the infor mation that aged care
service providers needed to understand to care for them effectively while in the context
of this report of stage two, service providers have elaborated on the way in which the
education of those in the aged care industry might proceed.
The complimentary perspectives of GLBTI seniors and aged care service providers
provide a strong foundation for the future development of an action plan (see appendix
4) to create GLBTI-friendly aged care services that operate within an aged care industry
which genuinely celebrates diversity.
__________________________________________________________________________________©
2009 Matrix Guild Victoria Inc
Permission to speak
66
_____________________________________________________________________
Conclusion
The
My People
and
Permission to Speak
reports have presented the experiences of 19
GLBTI seniors receiving aged care services and 36 aged care services providers
regarding GLBTI-friendly aged care services in Victoria. These participants provided
rich descriptions of their experiences and their suggestions for change. Consequently,
the reports do not seek to generalise about the entire population of aged care services.
Rather, the intent of stages one and two of the project is to provide evidence of the
experiences of GLBTI seniors in aged care services in Victoria and offer practical
strategies for change.
No previous studies in Australia have sought feedback from service providers and
recipients to provide information that might feed into the development of a plan to
create GLBTI-friendly aged care services. The Matrix Guild Victoria Inc and Vintage
Men Inc program has generated interest in the media, discussion in the community
and debate amongst aged care service providers and within the GLBTI community.
This level of attention has increased the visibility of GLBTI seniors and raised serious
concerns about their experiences in aged care services.
We live in an ageist society in which seniors are unseen and unheard and considered
to be asexual. Given that aged care ser vice providers have not been educated around
the needs of GLBTI seniors it is not surprising that their views reflect the ageism of
society. The vulnerability of some GLBTI seniors and their dependency on aged care
services demands that service providers must take a lead role in creating GLBTI-
friendly spaces. This process needs to take place in collaboration with gover nment,
GLBTI and aged care organisations, GLBTI seniors themselves and other key
stakeholders.
Many of the strategies for change described in this report will take years to achieve. In
the interim GLBTI seniors and service providers have vividly described serious
discrimination which is currently taking place. Consequently, there is an imperative to
act quickly to create change.
__________________________________________________________________________________
© 2009 Matrix Guild Victoria Inc
Permission to speak
67
_____________________________________________________________________
Appendix 1: Core issues in relation to GLBTI seniors
1. The impact of historical experiences of discrimination:
The current generation of GLBTI seniors was
coming of age at a time when their sexual/gender identity could result in enforced medical ‘cures’,
imprisonment or loss of family, employment and friends. Consequently, they have special needs which
need to be understood by aged care service providers. In particular, some GLBTI seniors: have never
experienced a time when they have felt safe disclosing their sexual/gender identity; revisit past
discriminatory experiences when encountering discrimination and consequently feel upset, anxious and
depressed; have learned that they need to be assertive to prevent discrimination; and often have a network
of ‘chosen’ family or friends rather than genetic family ties, although some may have few social
connections.
2. Invisibility as an impact of current discrimination:
Some GLBTI seniors closet their sexual/gender
identity in aged care services through fear of discrimination. They are aware of the risks because they have:
experienced discrimination in aged care services; heard reports about discrimination in these and related
services; witnessed discriminatory responses from aged care service providers to GLBTI people profiled in
the media. Consequently they: fear a diminished standard of care or deterioration in their relationships with
their carers; fear the resignation of valued home carers; believe that aged care service providers do not
expect them to be sexual or GLBTI; and believe that many aged care service providers do not understand
what GLBTI or GBLTI culture means and therefore cannot meet the needs of GLBTI seniors.
3. The impact of identity concealment:
GLBTI seniors who feel unable to disclose their sexual/gender
identity may: feel unable to be themselves and feel devalued or depressed; experience stress and pressure
from maintaining a façade of heterosexuality; have unmet care needs; and have limited opportunities for
sexual expression.
4. The impact of inadvertent visibility:
Some GLBTI seniors are exposed to discrimination from staff, co-
clients and visitors because they are unable to hide their sexual/gender identity. These seniors, who require
protection in aged care services, may include: transsexuals who do not pass as a man or a woman; cross-
dressers who do not have the opportunity to cross-dress in privacy; those who have a demonstrative
relationship with their same-sex partner; men who are HIV positive and are therefore presumed to be gay;
and seniors with dementia who have lost their capacity to assess when and where it is safe to disclose their
sexual/gender identity.
5. The impact of dementia:
Some GLBTI seniors have dementia and need: staff to understand that the grief
and loss involved in having a same-sex partner with dementia is no less than that experienced by a
heterosexual couple; to have their relationships recognised by aged care service providers, other clients and
families; to be protected from discrimination by co-clients with dementia; to be supported to provide
informed consent relating to sexual expression; and to be cued around gender/sexual identity if required.
6. Enabling sexual and cultural expression:
Sexual and cultural expression is important for the mental
health of GLBTI seniors. Sexual expression may involve: physical touch such as holding hands, hugging,
kissing; contact with partners and private time together; sexual intercourse or masturbation; and use of sex
toys and sexually explicit material such as magazines, DVDs and book. Cultural expression may involve:
making connections with the GLBTI community, including being with other GLBTI people, reading
GLBTI community magazines, watching GLBTI television programs, attending special festivals/meetings
and events; and dressing in clothing that expresses their sexuality/gender.
7. Inadequate standards of care:
Some aged care services discriminate against GLBTI seniors by failing to
create GLBTI-friendly services. Characteristics of these services include: staff being unaware of their legal
responsibilities regarding discrimination; staff not being held to account if discrimination occurs; a lack of
staff guidance in the form of organisational policies, education and leadership around the care of GLBT
seniors; the provision of a diminished standard of care to GLBTI seniors; staff failing to protect GLBTI
seniors from discrimination by co-clients and visitors in shared services; restricting opportunities for sexual
expression; allowing the values and beliefs of aged care service providers to govern the care delivered to
GLBTI seniors; and withdrawing physical contact from gay men in the belief that HIV/AIDS will be
contracted.
8. Achieving a safe environment:
A positive response to the disclosure of sexual/gender identity can result
in GLBTI seniors feeling understood, valued and safe. A positive response can be achieved when aged care
services create GLBTI-friendly aged care services by: affirming the legitimacy of GLBTI seniors’
sexual/gender identity; creating opportunities for dialogue with GLBTI seniors around their care needs;
understanding the importance of sexual expression and providing GBLTI seniors with opportunities for
sexual expression to occur; and valuing the intimate relationships and friendships of GLBTI seniors.
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Permission to speak
68
_____________________________________________________________________
Appendix 2: Media interest register
Date Type Title Details
30/08
JOY FM Well well well Gay & lesbian radio- HIV
/2007
and men's health segment
29/05
Joy FM Well well well Gay & lesbian radio- HIV
/2008
and men's health segment
14/03
The Age Newspaper The cost of living: HIV/AIDS Article by Julia Medew
/2008
3/05/
The Age Newspaper A lifetime wait for change Article by Carol Nader
2008
31/07
BNEWS Care for older gays Article by Andie Noonan
/2008
JOY FM Been there done that
15/8/
Media release-LaTrobe
Gay seniors go back to the closet as
Web based media release
2008
University
age care providers shun their needs
by Adrienne Jones
13/08
Pinke.biz (UK) Web based article by
/2008
Eleni Henderson
13/08
Sydney Star Observer Senior gays 'missing out' Newsprint by Andie
/2008
Noonan
20/08
Lesbian Life (USA) LGBT seniors in aged care services
Web based article
/2008
face discrimination
20/08
Same Same Report damms GLBTI aged care Web based article
/2008
19/09
Science Alert Australia New
Gay seniors shunned by carers Web based article
/2008
Zealand
17/09
Accessibility Gay Seniors Feel Impact Of Poor
Web based article
/2008
Aged Care Options
24/09
MCV GLIBT seniors face discrimination Article by Rachael Cook
/2008
19/09
Iconocast (USA) Gay seniors shunned by carers Web based article
/2008
17/09
Australian Ageing Agenda GLBTI discrimination remains a
Web based article
/2008
problem
28/09
JOY FM Allegro Non Troppo Gay & lesbian radio-
/2008
classical music segment
8/10/
Life Matters - ABC radio ABC radio Radio national interview
2008
with Richard Aedy
Octo
Burondoora Leader Newspaper
ber
1/10/
Aged care crisis.com
Gay seniors feel impact of poor aged
Sydney Star Observer -
2008
care options
Ani Lamont
1/10/
Aged Care Guide
Gays claim discrimination in aged
Web based article
2008
care services
1/10/
Elder Abuse Spotlight GLBTI seniors discriminated Web based article by
2008
Travis de Jonk
__________________________________________________________________________________© 2008
Matrix Guild Victoria Inc
Appendix 3: List of resources
Aged & Community Care Victoria:
A peak body for aged care in Victoria which exists to
promote, encourage and assist the health and care needs of the aged and community care
clients and to provide leadership in the aged and community care sector.
http://www.accv.com.au/
Aged Care Complaints Investigation Scheme
(1800 550 552):
Available to anyone who
wishes to provide information or make a complaint about an Australian Government-
subsidised aged care service, including nursing homes, hostels, community aged care
packages and extended aged care at home.
Aged Care Standards and Accreditation Agency:
The independent body responsible for
managing the
accreditation
residential age care facilities to improve service quality.
(http://www.accreditation.org.au/)
ALSO Foundation (9827 4999):
Works to enhance the lives of Victoria's diverse GLBT
communities to create and celebrate a diverse, strong, safe and inclusive GLBTIQ community
that contributes to and is respected by broader communities. (http://www.also.org.au/).
Alzheimer’s Australia Hotline (1800 100 500):
The peak body providing support and
advocacy for the Australians living with dementia.
Carers Victoria (1800 242 636):
A state-wide voice for family carers, representing and
providing support to carers in the community for information, advice, personal support, and
to access counselling. http://www.carersvic.org.au/index.htm
Community Visitors Program
(1800 136 829):
A community visitor is a trained volunteer
who visits a range of residential services (including aged care) to identify, monitor and
resolve issues and protect the rights and interests of people with a disability.
http://www.publicadvocate.vic.gov.au/Services/Community-Visitors.html
Council on The Ageing
: An independent consumer organisation run by and for senior
Australians to protect and promote the well-being of all seniors. http://www.cota.org.au/
Gay and Lesbian Health Victoria
: A website and clearinghouse that provides news and
information of particular interest to the health and well-being of GLBTI people in Victoria.
Gay and Lesbian Issues and Psychology Review:
In 2006 this journal was the first peer-
reviewed journal in Australian to focus on GLBTI Ageing. The issue was edited by Dr Jo
Harrison and Dr Damien W Riggs and is available on the Rainbow Visions site, at:
(http://www.rainbowvisions.org.au/GLIP_Review_Vol2_No2.pdf).
Inter
Section Melbourne (9471 4878):
An activist group with a web-based presence
which takes action in relation to GLT ageing including advocating policy change. It also acts
towards the development of programs to make local governments aware of the issues in their
communities, including the issues for older gay men and lesbians.
(http://www.zip.com.au/~josken/ageing.htm).
Matrix Guild Victoria Inc. ( 9532 4030):
Founded by and for the benefit of lesbians over
forty years of age. The Guild is committed to the support of appropriate care and
accommodation choices and alternative lifestyle options for older lesbians in Victoria.
(http://www.matrixguildvic.org.au).
National Aged Care Advocacy Line
(1800 700 600):
A national program promoting the
rights of older people receiving Australian Government-funded aged care services to the
community. The advocacy line can provide advice about rights; assist seniors to exercise their
rights and work with the aged care industry to encourage policies and practices which protect
consumers.
National GLBT Health Alliance:
Established by a number of organisations working in the
area of GLBT health research, programs and services to advocate on behalf of GLBT
communities at a national level, with politicians, researchers, funders, and in the
media.
(http://glbthealth.org.au/)
Rainbow Visions:
A coalition of individuals and groups who initiate and support actions that
contribute to making the Hunter region a healthier , more enjoyable, rewarding and culturally
rich place for GLBTIQ people.
(
http://www.rainbowvisions.org.au/index.html).
Seniors Rights Victoria
(1300 368 821):
A free service that has been established to help
prevent elder abuse and safeguard the rights, dignity and independence of older Victorians.
The service provides telephone information and referral, advocacy and support, legal
services, community and professional education.
Victorian AIDS Council/Gay Men’s Health Centre (9865 6700):
A community health
service which aims to improve the health and social and emotional well-being of the
Victorian HIV positive and Gay, Lesbian, Bisexual and Transgender communities. In
particular, we are invested in bring the AIDS epidemic to an end.
(http://www.vicaids.asn.au/content/default.asp).
Vintage Men (0419 341 547):
A social and suppor t group for mature gay and bisexual men
and their friends. (www.geocities.com/vintagemen).
Appendix 4.
Draft Strategic options to encourage the development of GLBTI-friendly
aged care serv ices in Victoria
This report explored the experiences of GLBTI seniors and aged care service providers and
their perspectives on strategies to create GBLTI-friendly aged care services. The following
pages provide draft strategic options recommended by program participants. These
recommendations relate to eight themes derived from the analysis of the two projects
undertaken and include:
1. Establish a lobby group
2. Implement immediate advocacy and support
3. Educate aged care service providers
4. Support change champions
5. Educate the community
6. Empower GLBTI seniors and their advocates
7. Support the development of GLBTI-specific services
8. Conduct further research.
The goal of each recommendation is presented before listing the objective and tasks
undertaken to achieve each goal.
1. Establish a lobby group
Aim:
To ensure a successful response to the serious concerns voiced in this report by
identifying powerful allies who can support the development of GLBTI-friendly aged care
services. Actions could include:
1.1. Invite key stakeholders to participate in a lobby group
1.1.1. Identify key stakeholders
1.1.2. Prioritise a list of actions responding to this report
1.1.3. Implement actions
1.2. Increase government responsiveness to the needs of GLBTI seniors by liaising
with government to:
1.2.1. Support strategies to create GLBTI-friendly aged care services
1.2.2. Include sexual and gender identity education and the needs of GLBTI seniors
in the training of aged care service providers
1.2.3. Explicitly refer to sexual and gender identity and the needs of GLBTI seniors
in the Standards and Guidelines for Residential Aged Care Services
1.2.4. Identify processes to monitor compliance of aged care services with
antidiscrimination legislation relating to GLBTI seniors
1.2.5. Support strategies to educate the community
1.2.6. Support strategies to empower GLBTI seniors and their advocates
1.2.7. Fund further research relating to GLBTI seniors
1.2.8. Provide support and education to mainstream organisations with the capacity
to support GLBTI seniors including: Seniors Rights Victoria; The Community
Visitors Program at the Office of the Public Advocate; and the Aged Care
Standards and Accreditation Agency.
1.3.
Further investigate options for the development of GLBTI-specific aged care services
as one strategy to create GLBTI-friendly aged care services
1.4.
Lobby for research funding to gather further evidence about the needs of GLBTI
seniors and the effectiveness of interventions to create GBLTI-friendly aged care
services
1.5.
Support the development of policies and program guidelines specific to the needs of
GLBTI seniors.
2. Develop processes for immediate advocacy and support
Aim
: To provide immediate relief to GLBTI seniors experiencing discrimination in aged care
services.
2.1.
Identify existing mainstream advocacy and support organisations that are positioned
to support GLBTI seniors in aged care services such as: Seniors Rights Victoria; The
Community Visitors Program at the Office of the Public Advocate; and the Aged
Care Standards and Accreditation Agency.
2.2.
Provide these existing groups with education and support around the needs of GLBTI
seniors
2.3.
Support change champions (see point 4)
3. Educate aged care service providers
Aim:
To create aged care services in which GLBTI seniors have permission to speak about
their sexual or gender identity. This will be suppor ted by providing education to aged care
service providers which takes into account the low literacy and high turnover of staff in some
services. Sharing GLBTI seniors’ stories could be employed to assist aged care service
providers to understand situations they may not have encountered. Education could also seek
to provide aged care service providers with permission to speak about their values and beliefs
and acknowledge any discomfort around sexuality or intimacy. Educational content could
include:
3.1. Give aged care service provider permission to discuss sexual and gender identity
3.1.1. Disseminate copies of this report and the
My people
report
3.1.2. Discuss traditional responses to sexual expression
3.1.3. Discuss values and beliefs around sexual expression
3.1.4. Clarify sexual boundaries between clients and staff
3.1.5. Explore beliefs around the use of libido suppressants
3.2. The importance of sexual and gender identity and ageing
3.2.1. What sexual and gender identity means
3.2.2. How sexual and gender identity changes with age
3.3. The legislative requirements/guidelines governing the care of GLBTI seniors:
3.3.1. Anti-discrimination legislation including:
3.3.1.1.The Charter of Human Rights and Responsibilities (2006)
3.3.1.2.The Equal Opportunity Act (1995)
3.3.1.3.The Statute Law Amendment (Relationships) Act (2001)
3.3.2. The relationships between anti-discrimination legislation and aged care
legislation including:
3.3.2.1.The Aged Care Act (1997)
3.3.2.2.The Guidelines for the Home and Community Care Program National
Service Standards (2003)
3.3.2.3.The Standards and Guidelines for Residential Aged Care Services (2006)
3.3.3. How discrimination might manifest in practice
3.3.4. The legal consequences of discrimination
3.3.5. The legal responsibility to protect GLBTI seniors from discrimination
3.3.6. The importance of guiding staff with organisational policies, education and
leadership relating to the needs of GLBT seniors
3.3.7. The legislation relating to sexual encounters between staff and clients
3.3.8. The legislation regarding the use of chemical restraints such as Androcur
3.4. What sexual and gender identity means to GLBTI seniors
3.4.1. Beliefs and perceptions in the general community regarding GLBTI seniors
3.4.2. How sexual and gender identity is expressed by GLBTI seniors
3.4.3. How sexual and gender identity differs between heterosexual and GLBTI
seniors
3.4.4. How to create dialogue between GLBTI seniors and staff
3.5. The concept of sexual and gender identity as culture for GBLTI seniors
3.5.1. Differentiation between sex and culture
3.5.2. The importance of cultural connections
3.5.3. The need for staff to demonstrate cultural competency and provide safety
3.5.4. The impact of cultural isolation
3.6. The importance of sexual and cultural expression for health
3.6.1. The need to provide opportunities for sexual and cultural expression
3.6.2. The value of intimacy and touch and friendships
3.6.3. The need for privacy in shared services and at home
3.6.4. The consequences of prohibiting sexual and cultural expression
3.6.5. The correlation between dependency on services/family and reduced
opportunities for sexual and cultural expression
3.6.6. The negative impacts of identity concealment
3.6.7. The importance of intimacy and touch
3.6.8. The reasons why identity concealment occurs
3.6.9. The benefits of sexual and cultural expression
3.7. The historical experiences of GLBTI seniors and implications for care
3.7.1. The legal, medical and societal responses to GLBTI people in the early 20
th
century
3.7.2. How past experiences of discrimination might affect the perceptions GLBTI
seniors have of themselves
3.7.3. The fears associated with disclosure
3.7.4. The importance of ‘chosen’ family or friends rather than genetic family ties
3.8. Strategies to develop GLBTI-friendly aged care services where seniors feel
understood, valued and safe:
3.8.1. Affirm the legitimacy of GLBTI seniors’ sexual or gender identity
3.8.2. Create opportunities for dialogue with GLBTI seniors around their care needs
3.8.3. Understand the importance of sexual and cultural expression and provide
GLBTI seniors with opportunities for sexual expression to occur
3.8.4. Value the intimate relationships and friendships of GLBTI seniors
3.8.5. Establish organisational systems and policies to support GLBTI seniors rather
than rely on individual staff members
3.9. Positive responses to the disclosure of sexual and gender identity
3.9.1. Ensure that GLBTI seniors play significant roles in decisions that impact on
them, as far as is possible. Ensure that their voices are heard; they are visible
and their preferences are sought
3.9.2. Responding to individuals rather than stereotypes
3.10. The impact of staff values and beliefs of service providers on GLBTI
seniors
3.10.1. Education which enables staff to explore their own values and beliefs and the
impacts of these on the care that they provide
3.10.2. The effects of community perceptions on aged care
3.11. The potential vulnerability of GLBTI seniors who are unable or choose
not to conceal their identity and therefore require additional protection
including:
3.11.1. Transsexuals who do not pass as a man or a woman
3.11.2. Cross-dressers who do not have the opportunity to cross dress in privacy
3.11.3. Those who have an open relationship with their same sex partner
3.11.4. Men who are HIV positive and are therefore assumed by staff to be gay
3.11.5. Seniors with dementia who have lost their capacity to assess when and where
it is safe to disclose their sexual or gender identity.
3.12. The needs of GLBTI seniors with dementia who require:
3.12.1. Staff to understand that the grief and loss involved in having a same-sex
partner with dementia is no less than that experienced by a heterosexual
couple
3.12.2. To have their relationships recognised by aged care service providers, other
clients and families
3.12.3. To be protected from discrimination by co-clients with dementia
3.12.4. To be supported to provide informed consent relating to sexual expression
3.12.5. To be supported to maintain their gender or sexual identity.
3.13. The needs of older gay men
3.13.1. Staff values, beliefs and stereotypes about being gay and being an older gay
man
3.13.2. The use of universal infection control guidelines and the fear of HIV/AIDS
3.13.3. The need for physical touch and intimacy
3.13.4. Strategies to protect gay men in shared services
3.13.5. Understanding the effects of dementia on the lives of gay seniors
3.14. The needs of older lesbians
3.14.1. Staff values, beliefs and stereotypes about lesbians and older lesbians
3.14.2. The historical role of women and lesbians including lesbian feminism
3.14.3. The barriers to sexual and cultural expression for older lesbians
3.14.4. Strategies to protect lesbians in shared aged care services
3.14.5. The effects of dementia for older lesbians
3.15. The needs of transgender seniors
3.15.1. Staff values, beliefs and stereotypes about seniors transsexuals and cross
dressers
3.15.2. The care needs of seniors who are male to female and female to male
transsexuals
3.15.3. The impact of the difficulty accessing gender reassignment surgery in the
early 20
century
th
3.15.4. The physical, emotional and psychological needs of seniors who are
transgender and the consequences of limited access to gender reassignment
surgery
3.15.5. Why some seniors cross dress and the consequences of prohibiting cross
dressing
3.15.6. The potential difficulty maintaining gender roles with ageing
3.15.7. The potential isolation for transgender seniors and the vulnerability that this
creates
3.15.8. Strategies to facilitate sexual and gender expression in shared services
3.15.9. The impact of dementia on the capacity to maintain gender identity
3.16. The needs of intersex seniors
3.16.1. Staff values, beliefs and stereotypes about who intersex seniors are
3.16.2. Understand the invisibility of intersex seniors and identify potential needs
4. Support change champions
Aim:
To improve the care provided to GLBTI seniors by supporting change champions who
seek to create GBLTI-friendly aged care services.
4.1.
Identify individual change champions including aged care service providers, GLBTI
seniors, families and advocates of GLBTI seniors
4.2.
Identify teams and organisations that are change champions
4.3.
Assess support needs
4.4.
Provide support and resources
4.5.
Identify strategies to recognise the leadership of change champions
4.6.
Share change stories with other potential change champions
5. Educate the community
Aim:
To reduce disparities for GLBTI seniors and increase their supports by providing
community education around the experiences and needs of GLBTI seniors.
5.1.
Clarify community values, beliefs and stereotypes around GLBTI seniors
5.2.
Identify resources to support community education
5.3.
Develop and implement education
5.4.
Target education program in rural communities and amongst heterosexual seniors
6. Empower GLBTI seniors and their advocates
Aim:
To enable GLBTI seniors and/or their advocates to understand and assert their rights in
aged care services.
6.1.
Develop accessible information on the rights of GLBTI seniors including:
6.1.1. Legislation relating to discrimination
6.1.2. What to do if advocacy is required
6.1.3. What to do if discrimination has occurred
6.1.4. How to protect oneself from homo/transphobia
6.2.
Seek feedback from GLBTI seniors on the information they require and the action
they have taken and ideas they have
6.3.
Provide educational information that could be given to service providers by GLBTI
seniors (or others on behalf of a senior who wishes to remain anonymous)
6.4.
Ensure that the voices of GLBTI seniors are heard and are involved in decision-
making which impacts on their lives, at all times.
7. Support the development of GLBTI-specific services
Aim:
To ensure that a range of GLBTI-friendly aged care services are available to GLBTI
seniors.
7.1.
Clarify what GLBTI-specific aged care services will be supported by GLBTI seniors
eg: residential aged care, community care, HIV/AIDS specific facility, advocacy
service or other agency
7.2.
Explore the symbolic significance of GLBTI-specific aged care services for GLBTI
seniors
7.3.
Where appropriate identify strategies to support GLBTI-specific aged care services
8. Conduct further research
Aim:
To promote further research in order to build on the body of evidence regarding the
needs of GLBTI seniors. New initiatives could include research relating to the:
8.1.
Historical experiences of GLBTI seniors
8.2.
Resilience and coping strategies developed by GLBTI seniors
8.3.
Community perceptions of GLBTI seniors
8.4.
Perceptions of aged care service providers
8.5.
Experiences of intersex seniors
8.6.
The experiences of change champions
8.7.
Issues for GLBTI seniors living in rural areas
8.8.
The content of training programs for aged care service providers related to sexual
and gender identity
8.9.
Use of medications to decrease libido in aged care services
8.10.
Expanding the current program to include all Australian states and
territories
8.11.
Explore further the meaning of GLBTI-friendly aged care services
References
AGE CONCERN (2002) Policy Position Paper: Issues facing older lesbians, gay men and
bisexuals. Access date: March 2008. Available at:
(
http://www.ageconcern.org.uk/AgeConcern/Documents/OLGMppp.pdf
)
AUSTRALIAN INSTITUTE OF HEALTH AND WELFARE (2002) Older Australia at a
glance. Canberra, Australian Institute of Health and Welfare, Commonwealth Department of
Health and Ageing
AUSTRALIAN MEDICAL ASSOCIATION (2002) Sexual diversity and gender identity.
Access date: March 2008. Available at:
(
http://www.ama.com.au/web.nsf/doc/WEEN-5GA2YX
)
AUSTRALIAN PRESCRIPTION PRODUCTS GUIDE (2007) Androcur CMI. Access date:
June 2008. Available at:
(
http://www.appgonline.com.au/drug.asp?drug_id=00075134&t=cmi
)
BARRETT, C., ANGEL, J., GILBERT, M., BOURAS, C., THOMPSON, K. &
SINGLETON, E. (2005a) Systematic processes for sustainable practice development.
Practice Development in Health Care,
4
,
5-13.
BARRETT, C., BORTHWICK, A., BUGEJA, S., PARKER, A., VIS, R. & HURWORTH, R.
(2005b) Emotional labour: Listening to the patient's story.
Practice Development in Health
Care,
4 213-223.
BAYER (2008) Control of libido in severe hypersexuality and/or sexual deviation in the adult
male.
Electronic medicines compendium.
Access date: June 2008. Available at:
(
http://emc.medicines.org.uk/emc/assets/c/html/DisplayDoc.asp?DocumentID=1808
)
BIRCH, H. (2004a) What about us? Positive ageing is also a GLBTI issue!
AAG Conference.
Melbourne.
BIRCH, H. (2004b) Ab
out
Time!: GLBT Seniors ALSO Matter. Melbourne, The ALSO
Foundation
BOURAS, C. & BARRETT, C. (2007) Strategies to enhance patient-centred care in a
cardiothoracic surgical unit.
Practice Development in Health Care,
6
,
150-164.
BRYER, L. (2004) Home-based services for older lesbians. A research report on behalf of
Matrix Guild Victoria Inc examining types of non-discriminatory, lesbian-sensitive support
services required by older, disadvantaged lesbians wishing to remain in their own homes.
CALLAN, M. (2006) Providing aged care services for the gay and lesbian community.
Australian Nursing Journal,
14
,
20.
CARR, W. & KEMMIS, S. (1986)
Becoming critical: Education, knowledge and action
research,
Burwood, Deakin University Press.
CHAMBERLAIN, C. & ROBINSON, P. (2002) The Needs of Older Gay, Lesbian and
Transgender People. Melbourne, RMIT University and the Centre for Applied Social
Research
COMMUNITY SERVICE AND HEALTH INDUSTRY SKILLS COUNCIL (2002).
Community Services Training Package.
Access date: May 2008. Available at:
(http://www.ntis.gov.au/Default.aspx?/trainingpackage/CHC02/download)
COOK-DANIELS, L. (1997) Lesbian, gay male, bisexual and transgendered elders: Elder
abuse and neglect issues.
Journal of Elder Abuse and Neglect,
9
,
35-49.
COUCH, M., PITTS, M., MULCARE, H., CROY, S., MITCHELL, A. & PATEL, S. (2007)
Tranznation: A report on the health and wellbeing of transgendered people in Australia and
New Zealand. Melbourne, Gay and Lesbian Health Victoria, Australian Research Centre in
Sex, Health and Society, La Trobe University
DE SAXE, M. & LOVETT, K. (2008) Inter~Section Melbourne.
Access date: March 2008. Available at: (
http://www.zip.com.au/~josken/inters3.htm
)
DEPARTMENT OF HEALTH AND AGEING AUSTRALIA (1997) Aged Care Act 1997:
Quality of care principles. Canberra, The Department of Health and Ageing Australia
DEPARTMENT OF HUMAN SERVICES VICTORIA (1988) Health Services Act 1988.
Canberra, The Department of Human Services.
DEPARTMENT OF HUMAN SERVICES VICTORIA (2003) Summary 2003 Supported
Residential Services (SRS) Census: Resident snapshot.
Access date: March 2008. Available at:
(
http://www.health.vic.gov.au/srs/downloads/resident_snapshot.pdf
)
DEPARTMENT OF HUMAN SERVICES VICTORIA (2004) Public sector residential aged
care policy: The Victorian Government's role in residential aged care services. Melbourne,
The Department of Human Services.
DEPARTMENT OF HUMAN SERVICES VICTORIA (2007) Ministerial Advisory
Committee on Gay and Lesbian Health. 2007.
Access date: March 2008. Available at: (
http://www.health.vic.gov.au/macglh/
)
DEPARTMENT OF HUMAN SERVICES VICTORIA (2008) HACC Facts.
Access date: March 2008. Available at:
(
http://www.health.vic.gov.au/hacc/hacc_victoria/facts.htm
)
DEPARTMENT OF HUMAN SERVICES (2008).
Because Mental Health Matters: A new
focus for mental health and wellbeing in Victoria.
Access date: May 2008. Available at:
(http://www.health.vic.gov.au/mentalhealth/reformstrategy/mhmatters-rep08.pdf)
HADFIELD, M. & HAW, K. (2001) 'Voice', young people and action research.
Educational
Action Research,
9
,
485-502.
HARRISON, J. (1999) A lavender pink grey power: Gay and lesbian gerontology in
Australia.
Australasian Journal on Ageing
, 18(1), 32-37.
HARRISON, J (2001) ‘It’s none of my business: Gay and lesbian invisibility in aged
care’ in Australian Occupational Therapy Journal Vol 48 pp142-145
Access date June 2008. Available at:
(
http://www.rainbowvisions.org.au/HarrisonAOTJournal48.pdf
)
HARRISON, J (2002a) ‘What are you really afraid of? Gay, lesbian, bisexual,
transgender and intersex ageing, ageism and activism’ in Word is Out March, pp1-11
Access date June 2008. Available at:
(
http://www.rainbowvisions.org.au/wordIsOut_by_JoHarrison.pdf
)
HARRISON, J (2002b) ‘LGBT Elders Gaining Ground in Australia’ in OutWord. American
Society on Aging. Vol 9 No 1 Summer. pp3-7
HARRISON, J. (2004a) ‘Discrimination and older gays: Surviving aged care’. in Equal Time.
NSW Anti-Discrimination Board. No 61 August.
Access date: March 2008. Available at:
(
http://www.lawlink.nsw.gov.au/lawlink/adb/ll_adb.nsf/vwFiles/ET%20Aug%2004%20.pdf/
$file/ET%20Aug%2004%20.pdf
)
HARRISON, J. (2004b) Towards the recognition of gay, lesbian, bisexual, transgender and
intersex (GLBTI) ageing in Australian gerontology
Annual Conference of the Australian
Lesbian Medical Association.
Leura, New South Wales.
HARRISON, J. (2004c) Towards the recognition of gay, lesbian, bisexual, transgender and
intersex ageing in Australian gerontology. Ph D thesis. School of Health Sciences, Division
of Health Sciences. The University of South Australia.
Access date: June 2008. Available at:
(
http://arrow.unisa.edu.au:8080/vital/access/manager/Repository/unisa:24955?query=Harriso
n%2c+J
)
HARRISON, J (2005a) ‘Pink, lavender and grey: Gay, lesbian, bisexual, transgender and
intersex ageing in Australian gerontology’ in Gay and Lesbian Issues and Psychology
Review. Vol 1, pp11-16. Access date: June 2008. Available at:
(
http://www.rainbowvisions.org.au/HarrisonGLIPReview.pdf
)
HARRISON, J. (2005b) Healthy ageing: What is it?
GLBT Health Ageing Forum ACON.
Access date: June 2008. Available at:
(
http://acon.org.au/community/index.cfm?doc_id=1737&cat_id=112
)
HARRISON, J. (2005c) Working Paper on Gay, Lesbian, Bisexual, Transgender and Intersex
Ageing and Discrimination Sydney, New South Wales Anti Discrimination Board. Access
date: June 2008. Available at:
(
http://www.lawlink.nsw.gov.au/lawlink/adb/ll_adb.nsf/pages/adb_glbti_consultation
)
HARRISON, J. (2006a) Coming out from the shadows and into the light: Gay, lesbian,
bisexual, transgender and intersex ageing-Celebrating diversity and taking action.
Australian
Association of Gerontology Conference.
Sydney.
Access date: June 2008 Available at: (
http://glhv.org.au/taxonomy/term/94
)
HARRISON, J. (2006b) Coming out ready or not! Gay, lesbian, bisexual, transgender and
intersex ageing and aged care in Australia: Reflections, contempor ary developments and the
road ahead.
Gay and Lesbian Issues and Psychological Review,
2
,
44-54. Access date: June
2008. Available at:
(
http://www.rainbowvisions.org.au/GLIP_Review_Vol2_No2.pdf
)
HARRISON, J. (2006c) OutWord Online: Insider's perspective on LGBT aging issues in
Australia. 2006. Access date: March 2008. Available at:
(
http://www.asaging.org/networks/lain/outword_online/2006/nov.cfm
)
HUGHES, M. (2006) Queer ageing.
Gay and Lesbian Issues and Psychological Review,
2
,
54-59.
HUGHES, M. (2007) Older lesbians and gays accessing health and aged-care services.
Australian Social Work,
60
,
197-209.
KEMMIS, S. & MCTAGGART, R. (2000) Participatory action research. In DENZIN, N. &
LINCOLN, Y. (Eds.)
Handbook of qualitative research.
London, Sage Publications.
LEONARD, W. (2003) Health and sexual diversity: A health and well-being action plan for
gay, lesbian, bisexual, transgender and intersex Victorians. Melbourne, Ministerial Advisory
Committee on Gay and Lesbian Health
MENTAL HEALTH ACT COMMISSION (2003).
Placed amongst strangers: Tenth biennial
report 2001-2003.
London. The Stationery Office.
MCFALL SULLIVAN, S. (2008) Five questions for David Cameron: An intersex elder's
view of aging. LGBT Aging Issues Network, OUTWORD. Winter 2008. Access date: June
2008. Available at:
(http//:www.asaging.org/networks/LAIN/outword-143.cfm)
MCNAIR, R., ANDERSON, S. & MITCHELL, S. (2001) Addressing health inequalities in
Victorian lesbian, gay, bisexual and transgender communities.
Health Promotion Journal of
Australia,
11
,
32-38.
NATIONAL HEATLH AND MEDICAL RESEARCH COUNCIL (2007) Australian Code
for the Responsible Conduct of Research Canberra, Australian Government
OSBORNE, D., BARRETT, C., HETZEL, C., NANKERVIS, J. & SMITH, R. (2002) The
wellness project: Promoting older peoples' sexual health. Melbourne, National Ageing
Research Institute
PATTON, M. (2002)
Qualitative research and evaluation methods,
London, Sage.
PITTS, M., SMITH, A., MITCHELL, A. & PATEL, S. (2006) Private lives: A report on the
health and wellbeing of GLBTI Australians. Melbourne, Gay and Lesbian Health Victoria,
The Australian Research Centre in Sex, Health and Society
QUAM, J. (1993) Gay and Lesbian ageing. Access date: March 2008. Available at:
(
http://www.cyfc.umn.edu/seniors/resources/gayaging.html
)
QUAM, J. & WHITFORD, G. (1992) Adaptation and Age-Related Expectations of Older
Gay and Lesbians Adults.
The Gerontologist,
32
,
367-374.
QUEENSLAND CORRECTIVE SERVICES (2006) Administration form - Androcur
treatment consent/information. Access date: June 2008. Available at:
(
http://www.correctiveservices.qld.gov.au/Resources/Procedures/Support_Services/document
s/spsfrmandrocurtreat.doc
)
RITCHIE, J. & SPENCER, L. (1994) Qualitative data analysis for applied policy research. In
ALAN, B. & ROBERT, B. (Eds.)
Analyzing qualitative data.
London, Routledge.
SANDELOWSKI, M. (1993) Rigor or rigor mortis: The problem of rigor in qualitative
research revisited.
Advances in Nursing Science,
16
,
1-8.
SELLERS, C. & ANGERAME, M. (2002) HIV/AIDS in older adults: A case study and
discussion.
AACN Clinical Issues,
13
,
5-21.
TESTRO GLADYS, J. (1997) Lesbian Health, Independence & Well Being Resource.
Melbourne, The Matrix Guild of Victoria
THE AGED CARE STANDARDS AND ACCREDITATION AGENCY LTD (2006)
Results and processes in relation to the expected outcomes of the accreditation standards.
Melbourne, The Aged Care Standards and Accreditation Agency Ltd. Access date: April
2008. Available at:
(http://www.health.gov.au/internet/main/publishing.nsf/Content/ageing-manuals-sgr-
sgrindex.htms and guidelines)
VICTORIAN EQUAL OPPORTUNITY AND HUMAN RIGHTS COMMISSION (2006)
Your right to rights: The Victorian Charter of Human Rights and Responsibilities explained.
Melbourne, Access date: April 2008
(http://www.humanrightscommission.vic.gov.au/human%20rights/default.asp#humanrights)
Equal Opportunity Act
(1995). Access date: April 2008. Available at:
(
http://www.austlii.edu.au/au/legis/vic/consol_act/eoa1995250/
)
Statute Law Amendment (Relationships) Act
(2001). Access date: April 2008. Available at:
(
http://www.austlii.edu.au/au/legis/vic/bill/slab20002000395/
)
WINTER, R. (2002) Truth or fiction: Problems of validity and authenticity in narratives of
action research.
Educational Action Research,
10
,
143-154.
WOLF, R. (1996) Understanding elder abuse and neglect.
Aging,
367
,
4-9.
YIN, R. (2003)
Case study research: Design and methods,
London, Sage.
YIN, R. (2004) Case study methods. COSMOS Corporation. Access date: March 2007.
Available at (http://www.cosmoscorp.com/Docs/AERAdraft.pdf).

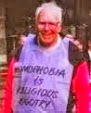
No comments:
Post a Comment